Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2019.3664?guestAccessKey=281ef30e-a44d-4fea-8fa1-bf8221d7aae2&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=112019
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.15834?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=112019
Gunshot Survivors Report Long-Term Physical, Mental Consequences
JAMA Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, NOVEMBER 20, 2019
Media advisory: To contact corresponding author Michael A. Vella, M.D., email Katie Delach at Katie.Delach@pennmedicine.upenn.edu. The full study, commentary and podcast are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2019.4533?guestAccessKey=2509a0b9-f751-40f1-b253-cda86055a584&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=112019
Bottom Line: Survivors of gunshot wounds reported negative outcomes years after being shot in this observational study. The study included about 180 gunshot wound survivors who were patients at an urban trauma center and who were surveyed by telephone up to 10 years following injury. Researchers report that, compared to before being shot, gunshot wound survivors had increased unemployment and alcohol and substance use, and nearly half screened positive for probable posttraumatic stress disorder. Gunshot wound survivors also scored lower on measures of physical health function and mental health compared with the general population. Limitations of the study include that most gunshot wound survivors couldn’t be contacted by telephone despite multiple attempts. Researchers also didn’t account for educational level and socioeconomic status, two potential factors that could influence the results. These findings suggest a role for long-term physical and mental health follow-up in this unique patient population.
Authors: Michael A. Vella, M.D., Perelman School of Medicine at the University of Pennsylvania, Philadelphia, and coauthors.
(doi:10.1001/jamasurg.2019.4533)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Barbra Streisand Featured in JAMA Podcast on Heart Disease in Women
JAMA
EMBARGOED FOR RELEASE: 2 P.M. (ET), MONDAY, NOVEMBER 18, 2019
Media advisory: The podcast and related articles linked below are being published to coincide with a session on cardiovascular disease in women at the American Heart Association’s Scientific Sessions 2019. To contact Dr. Bairey Merz email Sally Stewart at sally.stewart@cshs.org and to contact Barbra Streisand email Rupa Balasubramanian at rupa@fundamental-inc.com.
What The Podcast Is About: Oscar-winner, recording artist and filmmaker Barbra Streisand, who helped create a namesake Women’s Heart Center at Cedars-Sinai in Los Angeles, and Noel Bairey Merz, M.D., the center’s director, discuss cardiovascular disease in women, which often presents differently and may not be diagnosed.
Embed this link to provide your readers free access to the article that links to the podcast This link will be live at the embargo time https://edhub.ama-assn.org/jn-learning/audio-player/10.1001/jama.2019.18701
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.4241?guestAccessKey=11235ba9-494a-4f8d-8d8b-1150bf1ac6c8&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
Is Early Menopause Associated With Increased Risk of Cardiovascular Disease?
JAMA
EMBARGOED FOR RELEASE: 2 P.M. (ET), MONDAY, NOVEMBER 18, 2019
Media advisory: The full study is linked to this news release. This study is being released to coincide with a session on cardiovascular disease in women at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.19191?guestAccessKey=8f4e1663-2889-4cf6-bb95-dc63cceabfe4&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
What The Study Did: Whether natural premature menopause and premature menopause that results from surgery to remove a woman’s ovaries before age 40 are associated with increased risk of developing cardiovascular diseases was the focus of this observational study.
Authors: Pradeep Natarajan, M.D., M.M.Sc., of Massachusetts General Hospital in Boston, is the corresponding author.
(doi:10.1001/jama.2019.19191)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.16004?guestAccessKey=cd4bdfd7-bdec-4f1e-a285-a6787c2c93b0&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111919
Use, Costs for Medicare, Medicaid of Newer Heart Failure Medications
JAMA Cardiology
EMBARGOED FOR RELEASE: 8 A.M. (ET), MONDAY, NOVEMBER 18, 2019
Media advisory: The full study is linked to this news release. This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.4982?guestAccessKey=7b37195b-d33c-4ca0-a65d-7b388785619e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
What The Study Did: Medicare and Medicaid data were analyzed in this claims-based study to look at national patterns of use and costs for two newer medications approved to treat heart failure by the Food and Drug Administration in 2015.
Authors: Ambarish Pandey, M.D., M.S.C.S., of the University of Texas Southwestern Medical Center in Dallas, is the corresponding author.
(doi:10.1001/jamacardio.2019.4982)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
State Abortion Conscience Laws
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, NOVEMBER 19, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.15105?guestAccessKey=58f15a95-b9f5-482c-82d5-0faa969c1ceb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111919
What The Study Did: This study examined state laws that grant individuals and institutions rights to refuse participation in abortion based on their beliefs, that grant immunity from liability for such refusals, and that limit conscience rights when patient safety is at risk.
Authors: Nadia N. Sawicki, J.D., M.Be., of the Loyola University Chicago School of Law in Chicago, is the corresponding author.
(doi:10.1001/jama.2019.15105)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2019.3762?guestAccessKey=c4e4d2bb-571f-4375-a366-b06f75387cc7&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
Treatment of Migraine Pain in Randomized Clinical Trial
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, NOVEMBER 19, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.16711?guestAccessKey=ebc7732d-e666-466d-ada8-55e70734166b&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111919
What The Study Did: Adults experiencing a migraine of moderate or severe severity took the drug ubrogepant or placebo and reported if after two hours they were free of pain and of their most bothersome migraine-associated symptom in this randomized clinical trial.
Authors: Richard B. Lipton, M.D., of the Albert Einstein College of Medicine in Bronx, New York, is the corresponding author.
(doi:10.1001/jama.2019.16711)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Trial Compares Maternal Blood Loss With Immediate vs. Delayed Umbilical Cord Clamping
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, NOVEMBER 19, 2019
Media advisory: The full study and editorial are linked to this news release. A visual abstract is below.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.15995?guestAccessKey=4e792a47-fe42-4779-bc0e-eb7e18de8fee&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111919
What The Study Did: This randomized clinical trial compared maternal blood loss with immediate umbilical cord clamping (within 15 seconds after birth) versus delayed clamping (60 seconds after birth) in 113 women who had a scheduled cesarean delivery at term of 37 weeks or more.
Authors: Cynthia Gyamfi-Bannerman, M.D., M.Sc., of the Columbia University Irving Medical Center in New York, is the corresponding author.
Visual Abstract
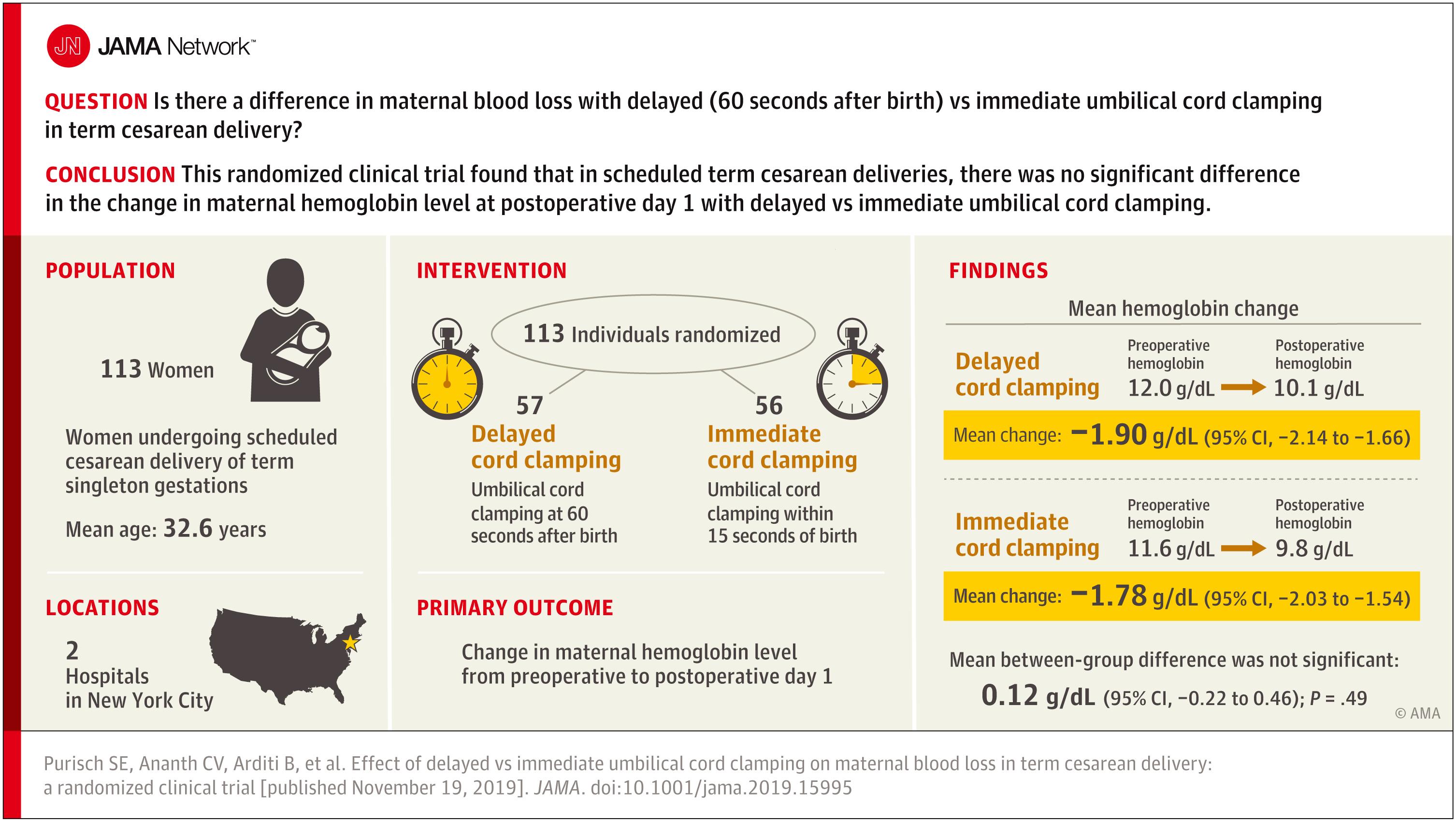
(doi:10.1001/jama.2019.15995)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Effects of HIV Self-Tests on Testing, Diagnosis
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 18, 2019
Media advisory: The full study and an editor’s note are linked to this news release. Also linked is a Special Communication article summarizing current guidelines and expert recommendations as part of a call for wider adoption of PrEP (preexposure prophylaxis) prescribing by frontline primary care physicians.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.5222?guestAccessKey=cc9a0299-6f7a-46fe-bdad-377ec3d24fab&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
What The Study Did: A 12-month randomized clinical trial used internet recruitment of men who have sex with men to evaluate the effects of providing self-tests for HIV to increase HIV testing and diagnosis among the men and people in their social networks.
Authors: Robin J. MacGowan, M.P.H., of the Centers for Disease Control and Prevention in Atlanta, is the corresponding author.
(doi:10.1001/jamainternmed.2019.5222)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Disparities in Care, Mortality Among Hospitalized Homeless Adults With Cardiovascular Conditions
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 1:30 P.M. (ET), MONDAY, NOVEMBER 18, 2019
Media advisory: The full study is linked to this news release. This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.6010?guestAccessKey=493acc16-47eb-468b-a5e8-665788f93fad&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
What The Study Did: Disparities in hospital care as measured by procedure rates and in-hospital death rates between homeless and nonhomeless adults hospitalized for cardiovascular conditions in New York, Massachusetts and Florida were examined in this observational analysis.
Authors: Rishi K. Wadhera, M.D., M.P.P., M.Phil., of Beth Israel Deaconess Medical Center and Harvard Medical School in Boston, is the corresponding author.
(doi:10.1001/jamainternmed.2019.6010)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.4357?guestAccessKey=8a0ad4d2-14d4-42c9-907e-a4f19ea9145f&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
Vaccine-Preventable Disease Outbreaks and State Legislative Proposals
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 18, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.4365?guestAccessKey=881efa13-09c0-4dbc-9db9-b96a437b23af&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
What The Study Did: This study explored how health is associated with legislative activity by examining whether outbreaks of vaccine-preventable diseases, such as measles, mumps, whooping cough and chickenpox, were associated with the introduction of legislation in states to change vaccine exemption laws.
Author: Neal D. Goldstein, Ph.D., M.B.I., of the Dornsife School of Public Health at Drexel University in Philadelphia, is the corresponding author.
(doi:10.1001/jamapediatrics.2019.4365)
Editor’s Note: The article contains conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Media advisory: This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.4973?guestAccessKey=b06230bd-3a86-488a-8745-876103c4037f&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
Did Medications Improve Outcomes in Patients With Heart Failure Who Had Heart Pump?
JAMA Cardiology
EMBARGOED FOR RELEASE: 8 A.M. (ET), MONDAY, NOVEMBER 18, 2019
Media advisory: The full study and editor’s note are linked to this news release. This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.4965?guestAccessKey=5d31d8ac-4fc2-4b5c-8dca-58a3c97d3b7b&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
What The Study Did: Researchers investigated if improved survival and quality of life were associated with neurohormonal blockade therapy (the drug classes angiotensin converting enzyme inhibitors or angiotensin receptor blockers, beta-blockers and mineralocorticoid antagonists) among 12,000 patients with heart failure who received a heart pump.
Authors: Nihar R. Desai, M.D., M.P.H., of the Yale University School of Medicine in New Haven, Connecticut, is the corresponding author.
(doi:10.1001/jamacardio.2019.4965)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2019.3876?guestAccessKey=bc6fc9c7-83e2-4aec-8fd5-e9f3f4119afb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111419
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.15374?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=111519
Comparing CPR Quality After Face-to-Face or Virtual Training
JAMA Cardiology
EMBARGOED FOR RELEASE: 8 A.M. (ET), SUNDAY, NOVEMBER 17, 2019
Media advisory: The full study is linked to this news release. This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.4992?guestAccessKey=b32dbe7e-fda0-49b4-b8f9-94f233c968b6&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111719
What The Study Did: Comparing the quality of cardiopulmonary resuscitation (CPR) delivered on manikins after face-to-face training with an instructor or virtual reality training using a smartphone app was the objective of the randomized clinical trial that included nearly 400 adults who attended a music festival in the Netherlands.
Authors: Joris Nas, M.D., of Radboud University Medical Center in Nijmegen, the Netherlands, is the corresponding author.
(doi:10.1001/jamacardio.2019.4992)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Media advisory: This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.4867?guestAccessKey=6d78abf6-02c7-45e3-be4d-1021eb5c2660&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111819
Experiences, Concerns of Patients With Heart Failure
JAMA Cardiology
EMBARGOED FOR RELEASE: 8 A.M. (ET), SUNDAY, NOVEMBER 17, 2019
Media advisory: The full study is linked to this news release. This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.4987?guestAccessKey=d45d7884-8a3c-4333-97a9-9f4b5e05bd0d&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111719
What The Study Did: Researchers sought to understand the experiences and perceptions of patients living with heart failure, as well as their familiarity and concerns regarding treatments for the condition, in this survey study of more than 400 patients.
Authors: Emily C. O’Brien, Ph.D., of the Duke Clinical Research Institute in Durham, North Carolina, is the corresponding author.
(doi:10.1001/jamacardio.2019.4987)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
How Did Outcomes Compare for Patients With Heart Failure After Telerehabilitation Program
JAMA Cardiology
EMBARGOED FOR RELEASE: 8 A.M. (ET), SUNDAY, NOVEMBER 17, 2019
Media advisory: The full study is linked to this news release. This study is being released to coincide with presentation at the American Heart Association’s Scientific Sessions 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.5006?guestAccessKey=3fb0d7ce-9ad4-44a8-bc0d-c2c313a3c1d8&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111719
What The Study Did: This randomized clinical trial investigated whether patients with heart failure in Poland would spend more time alive and out of the hospital if they participated in a mostly home-based, remote-monitored telerehabilitation program (one week in the hospital and nine weeks at home) compared to patients who received usual care.
Authors: Ewa Pietrowicz, M.D., Ph.D., of the Institute of Cardiology in Warsaw, Poland, is the corresponding author.
(doi:10.1001/jamacardio.2019.5006)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2019.4547?guestAccessKey=ac3c8d85-5f24-47da-8e44-4dafac02c61d&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111319
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2019.4620?guestAccessKey=8c836097-99b4-4700-83b1-0181e7d71795&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111319
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14078?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=111319
Is Association Between Hearing Loss, Impaired Cognition Present Earlier
JAMA Otolaryngology-Head & Neck Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, NOVEMBER 14, 2019
Media advisory: The full study, commentary and podcast are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/10.1001/jamaoto.2019.3375?guestAccessKey=3e4572b6-0e7a-4d5e-939b-f162fc58498b&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111419
What The Study Did: Researchers in this observational study looked at whether the association between hearing loss and cognitive impairment is present at earlier levels of hearing loss than previously believed.
Authors: Justin S. Golub, M.D., M.S., of New York-Presbyterian/Columbia University Irving Medical Center in New York, is the corresponding author.
(doi:10.1001/jamaoto.2019.3375)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.15360?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=111319
Analysis of Melanoma in US by Age Groups
JAMA Dermatology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, NOVEMBER 13, 2019
Media advisory: The full study and podcast are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamadermatology/fullarticle/10.1001/jamadermatol.2019.3353?guestAccessKey=e77e1f90-e7dd-49de-b4b6-7c9699c973cb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111319
What The Study Did: This study used registry data to determine annual rates of melanoma in pediatric, adolescent, young adult and adult age groups, and the findings suggest an apparent decrease among adolescent and young adults between 2006 and 2015 but increases in older adults.
Authors: Jennifer M. Gardner M.D., of the Seattle Cancer Care Alliance, is the corresponding author.
(doi:10.1001/jamadermatol.2019.3353)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Changing Weight-Loss Strategies, Attempts
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, NOVEMBER 13, 2019
Media advisory: To contact corresponding author Lu Qi, M.D., Ph.D., F.A.H.A., email Carolyn Scofield at cscofiel@tulane.edu. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.15219?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=111319
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
Bottom Line: The proportion of adults who tried to lose weight in the previous year increased from 1999 to 2016 but the findings of this observational study suggest the results may have been unsatisfactory. The analysis included data collected from about 48,000 adults ages 40 to 64 as part of a continuing national survey. The most commonly reported weight-loss strategies were eating less food, exercising and drinking more water, although increases were seen among those who attempted to lose weight in current measured body-mass index (BMI) and weight, as well as in the difference between current measured weight and adjusted self-reported prior year weight. The study has limitations to consider, including that self-perceived weight status and weight loss attempts and strategies were based on self-reported data.
Authors: Lu Qi, M.D., Ph.D., F.A.H.A., of Tulane University, New Orleans, and coauthors
(doi:10.1001/jamanetworkopen.2019.15219)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Opioid Overdose Deaths Among Younger Medicare Patients With Disability
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, NOVEMBER 15, 2019
Media advisory: To contact corresponding author Yong-Fang Kuo, Ph.D., email Christopher Smith Gonzalez at chrissmi@utmb.edu. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.15638?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=111519
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
Bottom Line: This observational study estimated the rate of opioid overdose deaths among Medicare enrollees younger than 65 who qualified for Medicare because of a disability. The study included more than 1.7 million of these enrollees in 2016 and 1,371 opioid overdose deaths. Researchers report those enrollees represented 14.9% of the Medicare population but they accounted for almost 81% of all opioid overdose deaths among all Medicare enrollees. The rate of opioid overdose deaths in this population increased from 57.4 per 100,000 in 2012 to 77.6 per 100,000 in 2016, and was greater among people with psychiatric diseases (such as depression, anxiety and bipolar disorder), substance use disorder (tobacco, alcohol or drug use) and chronic pain. Adults who had all three of these conditions had higher rate of opioid overdose death than those with none of the conditions. Limitations of the study include variations in the quality and accuracy of death certificate data associated with overdose.
Authors: Yong-Fang Kuo, Ph.D., of the University of Texas Medical Branch at Galveston, and coauthors.
(doi:10.1001/jamanetworkopen.2019.15638)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.15686?guestAccessKey=a29a5c95-7eea-4a79-b1db-a60469aaa318&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111219
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.14386?guestAccessKey=63cf07bd-47fa-487d-b10e-5ba17e1682d3&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111219
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.4221?guestAccessKey=015ce404-26a9-4c09-986b-0ec8043ea08b&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111119
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.4006?guestAccessKey=f342d7bf-78bc-493f-b48e-fd4feabc01fb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111119
How Likely Do You Think You Are to Develop Dementia?
JAMA Neurology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, NOVEMBER 15, 2019
Media Advisory: To contact corresponding author Donovan T. Maust, M.D., M.S., email Kara Gavin at kegavin@med.umich.edu. The full study is linked to this news release. This study is being released to coincide with presentation at the Gerontological Society of America 2019 Annual Scientific Meeting.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2019.3946?guestAccessKey=27c6954a-f71c-4ad3-b058-b21983ed5cc9&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111519
Bottom Line: A poll suggests almost half of adults ages 50 to 64 believe they’re likely to develop dementia. The survey included 1,019 respondents who were asked what risk they perceived and what potential risk-reducing measures they took. Of the participants, 48.5% said they were at least somewhat likely to develop dementia during their lifetime. Many participants reported strategies to try to maintain or improve memory that aren’t evidence based. Only a few participants (5.2%) had discussed potential ways to reduce dementia risk with their physician.
Authors: Donovan T. Maust, M.D., M.S., University of Michigan, Ann Arbor, and coauthors.
(doi:10.1001/jamaneurol.2019.3946)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Clinical Trial in Australia Tests Effectiveness of Naloxone by Nose vs. Injection for Opioid Overdose
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, NOVEMBER 13, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14977?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=111319
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: A randomized clinical trial in Australia tested whether a dose of naloxone administered through the nose was as effective as the same dose delivered by injection to reverse opioid overdose as measured by the need for a rescue dose delivered by injection 10 minutes after the initial treatment. The study included 197 clients at a medically supervised injecting center in Sydney where eligible patients (18 or older with a history of injecting drug use) are allowed to inject drugs under the supervision of clinically trained staff who watch for signs of overdose.
Authors: Paul Dietze, Ph.D., of the Burnet Institute in Melbourne, Australia, is the corresponding author.
(doi:10.1001/jamanetworkopen.2019.14977)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Use Changes After Recreational Marijuana Legalization
JAMA Psychiatry
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, NOVEMBER 13, 2019
Media advisory: To contact corresponding author Magdalena Cerdá, Dr.P.H., email Sasha Walek at Sasha.Walek@nyulangone.org. The full study, editorial and podcast are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2019.3254?guestAccessKey=3cd6baa3-b7f9-44f4-81bb-ea005c929794&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=111319
Bottom Line: How the legalization of recreational marijuana in some states was associated with changes in marijuana use and cannabis use disorder compared to other states from 2008 to 2016 was the focus of this study. Researchers used national survey data from nearly 506,000 participants in age groups from 12 to 17, 18 to 25, and 26 or older. The authors report that after the legalization of recreational marijuana, the proportion of respondents 12 to 17 reporting past-year cannabis use disorder increased from 2.18% to 2.72%. Also, the proportion of respondents 26 or older reporting frequent marijuana use increased from 2.13% to 2.62% and those reporting cannabis use disorder increased from 0.90% to 1.23%. No associations were found among those respondents 18 to 25. A limitation of the study is its reliance on self-reported marijuana use. The increases in use and risk of cannabis use disorder observed in this study are potential public health concerns.
Authors: Magdalena Cerdá, Dr.P.H., of the New York University School of Medicine, New York, and coauthors.
(doi:10.1001/jamapsychiatry.2019.3254)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Examining Muscle Relaxant Dose, Risk of Encephalopathy in Patients With CKD
JAMA
EMBARGOED FOR RELEASE: 10 A.M. (ET), SATURDAY, NOVEMBER 9, 2019
Media advisory: The full study is linked to this news release. This study is being released to coincide with presentation at Kidney Week 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.17725?guestAccessKey=da673453-54aa-42c7-9b1b-9e0c082c57d9&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110919
What The Study Did: Whether a higher or lower dose of the muscle relaxant baclofen was associated with 30-day risk of hospitalization with encephalopathy (defined as a main diagnosis of delirium, disorientation, transient alteration of awareness, transient ischemic attack or an unclear diagnosis of dementia) among newly prescribed patients with chronic kidney disease was the focus of this observational study with nearly 16,000 older adults.
Authors: Flory T. Muanda, M.D., Ph.D., of the Institute for Clinical Evaluative Sciences in London, Ontario, Canada, is the corresponding author.
(doi:10.1001/jama.2019.17725)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14861?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110819
Predicting Risk of Chronic Kidney Disease
JAMA
EMBARGOED FOR RELEASE: 2 P.M. (ET), FRIDAY, NOVEMBER 8, 2019
Media advisory: The full study and editorial are linked to this news release. This study is being released to coincide with presentation at Kidney Week 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.17379?guestAccessKey=46528152-dd1c-4a86-9b08-4bd9c325bf34&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110819
What The Study Did: Data from about 5 million people (with and without diabetes) in 28 countries were used to develop equations to help identify people at increased five-year risk of chronic kidney disease, defined as reduced estimated glomerular filtration rate (eGFR).
Authors: Josef Coresh, M.D., of the Johns Hopkins Bloomberg School of Public Health in Baltimore, is the corresponding author.
(doi:10.1001/jama.2019.17379)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14718?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110819
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14666?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110819
Did Vitamin D, Omega-3 Supplements Help Prevent Development, Progression of CKD in Adults With Type 2 Diabetes?
JAMA
EMBARGOED FOR RELEASE: 2 P.M. (ET), FRIDAY, NOVEMBER 8, 2019
Media advisory: The full study and editorial are linked to this news release. This study is being released to coincide with presentation at Kidney Week 2019.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.17380?guestAccessKey=52eec612-76c3-4d08-8c0b-496acbf71159&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110819
What The Study Did: Researchers in this randomized clinical trial investigated if supplementation with vitamin D or omega-3 fatty acids compared with placebo over five years helped prevent the development or progression of chronic kidney disease among adults with type 2 diabetes. The main outcome measure was change in the glomerular filtration rate that was estimated from serum creatinine and cystatin C.
Authors: Ian H. de Boer, M.D., M.S., of the University of Washington in Seattle, is the corresponding author.
(doi:10.1001/jama.2019.17380)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14561?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110619
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14689?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110619
Randomized Clinical Trial Focuses on Mailed HPV Self-Sampling Test Kits
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, NOVEMBER 6, 2019
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14729?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110619
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: This randomized clinical trial compared mailed at-home HPV self-sampling test kits with the usual care reminders patients receive about in-clinic screening for increasing the detection and treatment of cervical precancers and screening.
Authors: Rachel L. Winer, Ph.D., of the University of Washington in Seattle, is the corresponding author.
(doi:10.1001/jamanetworkopen.2019.14729)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Is Infection After Surgery Associated With Increased Long-Term Risk of Infection, Death?
JAMA Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, NOVEMBER 6, 2019
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2019.4539?guestAccessKey=15769b66-dd83-465f-a469-fab31ef44995&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110619
What The Study Did: Whether experiencing an infection within the first 30 days after surgery is associated with an increased risk of another infection and death within one year was the focus of this observational study that included about 660,000 veterans who underwent major surgery.
Authors: William J. O’Brien, M.S., of the VA Boston Health Care System, is the corresponding author.
(doi:10.1001/jamasurg.2019.4539)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Popular Flavors of JUUL Electronic Cigarettes Used by Teens
JAMA
EMBARGOED FOR RELEASE: 9 A.M. (ET), TUESDAY, NOVEMBER 5, 2019
Media advisory: To contact corresponding author Adam M. Leventhal, Ph.D., email Leigh Hopper at lhopper@usc.edu. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.17968?guestAccessKey=6cd13a73-46aa-460e-95c7-0cb2d9b66fdf&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110519
Bottom Line: Estimating the most common JUUL electronic cigarette flavors used by U.S. teenagers in 2019 was the focus of this study. Nationally representative survey data collected in 2019 from about 14,000 eighth, 10th and 12th graders were used, of whom nearly 19% reported vaping of any nicotine product in the past 30 days and 12.6% reported using JUUL e-cigarettes (7% in eighth grade, 15% in 10th grade and 16% in 12th grade). Data on flavor preference were available for 1,739 users of JUUL in the past 30 days. Researchers report mint was the most popular flavor among 12th and 10th graders, followed by mango. Among eighth graders, mango was the most popular, followed by mint. Among teens who used JUUL on 20 or more days in the past month, mint was the most popular flavor in all grades. The study findings raise questions about regulations and sales suspensions that exempt mint flavors as effective strategies to reduce e-cigarette use by adolescents. A limitation of the study is its generalizability only to JUUL users.
Authors: Adam M. Leventhal, Ph.D., University of Southern California, Los Angeles, and coauthors.
(doi:10.1001/jama.2019.17968)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.17144?guestAccessKey=0782f361-99d8-4820-ad96-39bcf4b82266&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110119
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3869?guestAccessKey=56c4b22b-ee5f-4594-bb23-c3813c9cccb1&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
Study Reports High Use of Electronic Cigarettes Among US Students in 2019
JAMA
EMBARGOED FOR RELEASE: 9 A.M. (ET), TUESDAY, NOVEMBER 5, 2019
Media advisory: To contact corresponding author Karen A. Cullen, Ph.D., email Michael Felberbaum at Michael.Felberbaum@fda.hhs.gov or Stephanie Caccomo at Stephanie.Caccomo@fda.hhs.gov. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.18387?guestAccessKey=54b2dc7d-3855-4728-a522-573083a5d2cd&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110519
Bottom Line: About 1 in 4 high school students and 10% of middle school students in 2019 reported current use of electronic cigarettes based on nationally representative survey data from U.S. students in grades six to 12. The findings suggest an estimated 4.1 million high school students and 1.2 million middle school students are using e-cigarettes in 2019. This study included about 19,000 participants in the 2019 National Youth Tobacco Survey to estimate how common e-cigarette use is among students including current use (past 30 days), frequent use (20 or more days in the past 30 days), usual e-cigarette brand, and the use of flavored products. Researchers report an estimated 27.5% of high school students and 10.5% of middle school students reported current e-cigarette use, and of those users, an estimated 34% of high school students and 18% of middle school students reported frequent use. JUUL was reported by 59.1% of high school students and 54.1% of middle school students as their usual brand of e-cigarettes in the past 30 days. Among current e-cigarette users who didn’t use other tobacco products, an estimated 72% of high school students and 59% of middle school students used flavored e-cigarettes, with fruit, menthol or mint, and candy, desserts, or other sweets being the most commonly reported flavors. Limitations of the study to consider include the 66% response rate to the survey because tobacco use may differ among those who participated in the survey and those that didn’t.
Authors: Karen A. Cullen, Ph.D., U.S. Food and Drug Administration, Silver Spring, Maryland, and coauthors.
(doi:10.1001/jama.2019.18387)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Investigating Childhood Stress Association With Blood Indicator of Chronic Inflammation
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 4, 2019
Media advisory: The full study and editorial are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3875?guestAccessKey=b2602038-150d-447c-895f-e6b420c8c2a5&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
What The Study Did: Researchers looked at whether exposure to adverse experiences, stress, and violence among 1,400 children in the United Kingdom was associated at age 18 with elevated levels in the blood of an indicator of chronic inflammation.
Author: Line Jee Hartmann Rasmussen, Ph.D., of Duke University in Durham, North Carolina, is the corresponding author.
(doi:10.1001/jamapediatrics.2019.3875)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
How Many NCAA Team Doctors, Trainers Are Women, Men?
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 4, 2019
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.5092?guestAccessKey=f3b1584d-e73a-4816-b561-71c771fdf7ed&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
What The Study Did: Researchers used the NCAA member directory to gather data to determine the distribution of women and men among head physicians and athletic trainers for teams in Divisions I, II and III in the 2018-2019 academic year.
Authors: Caitlin Lewis, M.D., of the Cleveland Clinic in Garfield Heights, Ohio, is the corresponding author.
(doi:10.1001/jamainternmed.2019.5092)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Association of Canadian Provincial Bans on Electronic Cigarette Sales to Minors, Use
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 4, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3912?guestAccessKey=46d9fcc3-a681-43df-b969-3a19566e5b8b&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
What The Study Did: This study investigated how Canadian provincial bans on electronic cigarette sales to minors were associated with changes in their e-cigarette use.
Author: Hai V. Nguyen, Ph.D., of Memorial University of Newfoundland, in St. John’s, Canada, is the corresponding author.
(doi:10.1001/jamapediatrics.2019.3912)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
30-Day Death Rates After Emergency Department Visits
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 4, 2019
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.4866?guestAccessKey=99de9e55-1910-4dd4-b8e5-f0164ccd08fa&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
What The Study Did: Researchers used Medicare data from 2009 to 2016 to see how 30-day death rates associated with emergency department visits have changed.
Authors: Laura G. Burke, M.D., M.P.H., of the Beth Israel Deaconess Medical Center in Boston, is the corresponding author.
(doi:10.1001/jamainternmed.2019.4866)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Evaluating Mind-Body Therapies for Opioid-Treated Pain
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 4, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.4917?guestAccessKey=56d96cb5-7a1b-4a3c-b5e2-b6295ee9dcca&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
What The Study Did: Mind-body therapies include things like meditation, hypnosis, relaxation and cognitive behavioral therapy. This study combined results from dozens of other studies to evaluate how mind-body therapies were associated with pain and opioid-related outcomes among adults using opioids for pain.
Authors: Eric L Garland, Ph.D., of the University of Utah in Salt Lake City, is the corresponding author.
(doi:10.1001/jamainternmed.2019.4917)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2019.3774?guestAccessKey=e00bf380-85b8-4c4e-9431-cd63f17993b3&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
Emergency Department Admissions of Children for Sexual Abuse
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, NOVEMBER 4, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3988?guestAccessKey=23d62a86-e9fd-4da2-a7eb-4bf038b9ee89&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110419
What The Study Did: This study analyzed emergency department admissions of children for sexual abuse between 2010 and 2016 using a nationwide database of emergency visits and U.S. Census Bureau data.
Authors: Jesse J. Helton, Ph.D., of St. Louis University in Missouri, is the corresponding author.
(doi:10.1001/jamapediatrics.2019.3988)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14393?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110119
STD Crowd-Diagnosis Requests on Social Media
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, NOVEMBER 5, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.14390?guestAccessKey=04d5272e-2067-4f91-b210-8fca1223cd20&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=110519
What The Study Did: Online postings seeking information on sexually transmitted diseases (STDs) on the social media website Reddit were analyzed to see how often requests were made for a crowd-diagnosis and whether the requested diagnosis was for a second opinion after seeing a health care professional.
Authors: John W. Ayers, Ph.D., M.A., of the University of California, San Diego, is the corresponding author.
(doi:10.1001/jama.2019.14390)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14401?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110119
Assessing Effect of Prescribing Fewer Opioids After Corneal Surgery
JAMA Ophthalmology
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, OCTOBER 31, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaophthalmology/fullarticle/10.1001/jamaophthalmol.2019.4432?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=103119
What The Study Did: What the association is between decreasing the number of opioid tablets prescribed to patients after corneal surgery and their opiod use and pain control was the focus of this observational study.
Authors: Maria A. Woodward, M.D., M.Sc., of the University of Michigan in Ann Arbor, is the corresponding author.
(doi:10.1001/jamaophthalmol.2019.4432)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14517?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110119
ADHD Across Racial/Ethnic Groups
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, NOVEMBER 1, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14344?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=110119
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: This study of patients from diverse racial/ethnic backgrounds who received care at the Kaiser Permanente Northern California health system looked at how common attention-deficit/hyperactivity disorder (ADHD) diagnoses were over a 10-year period across seven racial/ethnic groups.
Authors: Winston Chung, M.D., M.S., of Kaiser Permanente Northern California in San Francisco, and Michael P. Milham, M.D., Ph.D., of the Child Mind Institute in New York, are the corresponding authors.
(doi:10.1001/jamanetworkopen.2019.14344)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Insurance Coverage Among Patients With Head/Neck Cancer After ACA
JAMA Otolaryngology-Head & Neck Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, OCTOBER 31, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/10.1001/jamaoto.2019.2724?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=103119
What The Study Did: Researchers investigated the association between the Affordable Care Act and changes in the percentage of patients with insurance among 130,000 people with head and neck cancer across varying socioeconomic and demographic backgrounds.
Authors: Neelima Panth, M.D., M.P.H., of the Duke University School of Medicine in Durham, North Carolina, is the corresponding author.
(doi:10.1001/jamaoto.2019.2724)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.13733?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=103019
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14386?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=103019
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3845?guestAccessKey=6bec5455-df06-45bf-89d7-44db7d042891&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3939?guestAccessKey=3cfb13d2-3d7f-4763-90bd-d1aec82bb2ca&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2019.4702?guestAccessKey=6c0b80f5-293b-4f90-ad1f-f50c066f1f5d&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
Childhood Cancer Survivors and Later Breast Cancer Risk
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 28, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3807?guestAccessKey=92330737-9acb-43ca-85ed-c07b1be7dfb5&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
What The Study Did: This study examined later breast cancer risk in childhood cancer survivors following radiation and chemotherapy treatment.
Author: Lena H. Veiga, Ph.D., of the National Cancer Institute in Bethesda, Maryland, is the corresponding author.
(doi:10.1001/jamapediatrics.2019.3807)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Did Banning Sugar-Sweetened Drinks at Work Cut Employee Consumption?
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 28, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.4434?guestAccessKey=c104b006-fa16-4100-824e-a4e9af86af07&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
What The Study Did: This study examined the effects of a workplace ban on sales of sugar-sweetened beverages on employee consumption and health.
Authors: Elissa S. Epel. Ph.D., of the University of California, San Francisco, is the corresponding author.
(doi:10.1001/jamainternmed.2019.4434)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
What Are Encounters With Biased Patients Like for Physicians?
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 28, 2019
Media advisory: The full study, commentary and podcast are linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.4122?guestAccessKey=547e97c5-3be3-462f-a79e-48d53f162de3&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
What The Study Did: A group of 50 nonwhite hospitalist attending physicians, internal medicine residents and medical students described their encounters with biased patients (ranging from patients refusing care to explicit racist, sexist or homophobic comments and belittling jokes) in this qualitative study to understand physicians’ perspectives on these encounters, which could help in the development of best practices and training programs at institutions as the clinical workforce becomes more diverse.
Authors: Alicia Fernandez, M.D., of the University of California, San Francisco, is the corresponding author.
(doi:10.1001/jamainternmed.2019.4122)
Editor’s Note: The article contains funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2019.4107?guestAccessKey=31572357-2b2d-4b00-ba8e-ff65e337922e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102419
Detection of Oral HPV DNA in Teen, Young Adult Females
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, OCTOBER 25, 2019
Media advisory: To contact corresponding author Nicolas F. Schlecht, Ph.D., email Annie Deck-Miller at annie.deck-miller@roswellpark.org. The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14031?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=102519
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
Bottom Line: Researchers tested for HPV DNA in oral rinse samples collected over 10 years from a group of sexually active females (ages 13 to 21) who were planning to or had received the vaccine that targets four types of HPV. HPV was detected in 6.2% of 1,259 participants at baseline but oral HPV detection became less likely with time since becoming sexually active. And, researchers report detection of the HPV types targeted by the vaccine was even less likely among those who received at least one dose of the vaccine compared with those who were fully unvaccinated. Study cohort characteristics include a population that had more sexual partners and an earlier initiation of sexual activity than other groups that have been studied. HPV is a common sexually transmitted infection that is associated with increased risk of some cancers, including in the oral cavity.
Authors: Nicolas F. Schlecht, Ph.D., of the Roswell Park Comprehensive Cancer Center, Buffalo, New York, and coauthors
(doi:10.1001/jamanetworkopen.2019.14031)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Length of Time in US Associated With Immigrants’ Opioid Use
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, OCTOBER 25, 2019
Media advisory: To contact corresponding author Brian D. Sites, M.D., M.S., email Audra Burns at Audra.Burns@hitchcock.org. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.13979?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=102519
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
Bottom Line: The more time first-generation immigrants spend in the United States the more likely it appears they will use prescription opioids. This analysis used nationally representative survey data on health services that include prescription medications and self-reported length of time spent in the country. Among an estimated 41.5 million adult immigrants living in the United States, 3.2 million (7.8%) use prescription opioids. Study authors report the rate of opioid use increased from 4.7% among new immigrants (less than five years in the U.S.) to 14.8% among long-standing immigrants (in the U.S. 15 years or more). Nonimmigrants were more likely to use prescription opioids compared with all first-generation immigrants (16.1% vs. 7.8%). The findings suggest uniquely American cultural factors may promote opioid use.
Authors: Brian D. Sites, M.D., M.S., Dartmouth-Hitchcock Medical Center, Lebanon, New Hampshire, and coauthors
(doi:10.1001/jamanetworkopen.2019.13979)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
How is Physical Activity Associated With Fracture Risk in Older Women?
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, OCTOBER 25, 2019
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.14084?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=102519
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: In this observational study of 77,206 postmenopausal women, researchers looked at how physical activity and sedentary behavior were associated with risk of fracture.
Authors: Jean Wactawski-Wende, Ph.D., of the University at Buffalo in New York, is the corresponding author.
(doi:10.1001/jamanetworkopen.2019.14084)
Editor’s Note: The article contains funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
How Did Weight-Loss Surgery Affect Long-Term Health Care Expenses?
JAMA Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, OCTOBER 30, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2019.3732?guestAccessKey=7aa8ca1a-316f-44b0-9239-5a3ae22cbfe6&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=103019
What The Study Did: This observational study of nearly 10,000 veterans with severe obesity compared health care expenditures for veterans who had weight-loss surgery with those who didn’t during up to 10 years of follow-up.
Authors: Matthew L. Maciejewski, Ph.D., of the Durham VA Medical Center in Durham, North Carolina, is the corresponding author.
(doi:10.1001/jamasurg.2019.3732)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Study Examines Fetal Exposure to Acetaminophen, Risk of Childhood ADHD, ASD
JAMA Psychiatry
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, OCTOBER 30, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2019.3259?guestAccessKey=83e36a6e-f239-43f0-9c6e-9983db4436d0&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=103019
What The Study Did: Umbilical cord blood samples were used to examine an association between fetal exposure to acetaminophen and risk of childhood attention-deficit/hyperactivity disorder, autism spectrum disorder and other developmental disabilities in a group of nearly 1,000 mother-child pairs.
Authors: Xiaobin Wang, M.D., M.P.H., Sc.D., of the Johns Hopkins University Bloomberg School of Public Health in Baltimore, is the corresponding author.
(doi:10.1001/jamapsychiatry.2019.3259)
Editor’s Note: The article contains funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Is Weight Loss Surgery Associated With a Reduced Risk of Skin Cancer?
JAMA Dermatology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, OCTOBER 30, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamadermatology/fullarticle/10.1001/jamadermatol.2019.3240?guestAccessKey=8d3a865d-9619-4640-a9ee-a47149039d91&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=103019
What The Study Did: Researchers investigated the association between weight loss surgery and a subsequent diagnosis of skin cancer, including melanoma, among 4,000 obese patients in Sweden, who had the surgery or received usual treatment.
Authors: Magdalena Taube, Ph.D., of the University of Gothenburg, in Gothenburg, Sweden, is the corresponding author.
(doi:10.1001/jamadermatol.2019.3240)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
How Common is Pain in Kids, Teens With ASD?
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 28, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3826?guestAccessKey=fdb5efdd-1bbf-460b-a122-d4e205eddc37&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
What The Study Did: Survey responses from parents were used to assess how often children and teens (ages 6 to 17) with autism spectrum disorders (ASD) had repeated or chronic physical pain in the previous 12 months compared to children without ASD.
Authors: Daniel G. Whitney, Ph.D., and Danielle N. Shapiro, Ph.D.,of the University of Michigan in Ann Arbor, are the authors.
(doi:10.1001/jamapediatrics.2019.3826)
Editor’s Note: The article contains conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Dementia, Alzheimer Disease in People With Down Syndrome
JAMA Neurology
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 28, 2019
Media Advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2019.3666?guestAccessKey=32ec26cb-4f2f-4cde-aca9-87927ec2c770&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102819
What The Study Did: Medicaid claims data in Wisconsin were analyzed to examine how common dementia and Alzheimer disease were in people with Down syndrome because clinical studies show them to be at higher risk and to have an earlier onset of dementia.
Authors: Eric Rubenstein, Ph.D., of the University of Wisconsin-Madison, is the corresponding author.
(doi:10.1001/jamaneurol.2019.3666)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Study Examines First Use of Flavored Tobacco Products
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, OCTOBER 23, 2019
Media advisory: The full study is linked to this news release and a visual abstract is below.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time: https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.13804?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=102319
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Associations between the first use of flavored tobacco products and subsequent use of those products were examined in this observational study based on nationally representative survey data of more than 38,400 youth and adults in the United States.
Authors: Andrea C. Villanti, Ph.D., M.P.H., of the University of Vermont in Burlington, is the corresponding author.
Visual Abstract:

(doi:10.1001/jamanetworkopen.2019.13804)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Increase in Older Adults in US Associated With Increase in Heart Disease Deaths
JAMA Cardiology
EMBARGOED FOR RELEASE: 1:05 A.M. (ET), WEDNESDAY, OCTOBER 30, 2019
Media advisory: To contact corresponding author Stephen Sidney, M.D., M.P.H., email Janet Byron at Janet.L.Byron@kp.org. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.4187?guestAccessKey=7c7fe675-8c73-4065-a36e-898696329c13&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=103019
Bottom Line: An increase in the number of U.S. adults 65 and older from 2011 to 2017 was associated with an increase in heart disease deaths in that age group despite a slowly declining heart disease mortality rate in the total population. Data from the U.S. Centers for Disease Control and Prevention and the Census Bureau were used to examine changes in heart disease deaths in combination with demographic changes in the population in this observational study. Authors report the 65-and-older population grew from 41.4 million to 50.9 million from 2011 to 2017, an increase of nearly 23%, while the adult population younger than 65 grew by only 1.7%. The overall mortality rate from all heart disease adjusted to account for differences in age declined 5% while the total number of deaths increased 8.5%, with 80% of the deaths among adults 65 and older. Deaths from all heart disease increased 5.7% from 2011 to 2017 among adults younger than 65 but increased 9.3% among those 65 and older. From 2011 t02017, the overall age-adjusted mortality rate from coronary heart disease decreased 14.9% but increased 20.7% from heart failure as the underlying cause. Limitations of the study include the potential misclassification of death certificate coding of heart failure and limitations of national surveillance data. The authors stress that with the number of adults 65 and older projected to increase another 44% in the U.S. from 2017 to 2030, innovative and effective approaches to prevent and treat heart disease are needed.
Authors: Stephen Sidney, M.D., M.P.H., of Kaiser Permanente Northern California, Oakland, and coauthors.
(doi:10.1001/jamacardio.2019.4187)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Increasing Google Searches for Marijuana Chemical Component CBD
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, OCTOBER 23, 2019
Media advisory: To contact corresponding author John W. Ayers, Ph.D., M.A., email Louise Canton at louise@elevatedsciencecommunications.com. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.13853?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=102319
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. Every Wednesday and Friday, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
Bottom Line: Google searches from 2004 through April 2019 were used to measure U.S. public interest in cannabidiol (CBD), a chemical component of marijuana. Searches from the United States that mentioned “CBD” or “cannabidiol” were stable from 2004 through 2014 before substantial increases in search volumes of almost 126% in 2017 compared with 2016 and 160% during 2018 compared with 2017. There were 6.4 million Google searches for CBD during April 2019 and year-over-year forecasted search volumes are expected to increase nearly 118% during 2019 compared with 2018. A limitation of this observational study is that Google searches may reflect interest in CBD rather than interest in its use. Researchers urge that attention to CBD be a public health priority because of the growing interest that surrounds it to understand who uses it and why, and to evaluate its effects and potential drug interactions.
Authors: John W. Ayers, Ph.D., M.A., University of California San Diego, and coauthors
(doi:10.1001/jamanetworkopen.2019.13853)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Is Parental Income During Childhood Associated With Kids’ Later Schizophrenia Risk?
JAMA Psychiatry
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, OCTOBER 23, 2019
Media advisory: The full study and editorial are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2019.2299?guestAccessKey=fe6e8805-e2de-4902-9c7b-06159dc53293&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102319
What The Study Did: Researchers analyzed data from everyone born in Denmark from 1980-2000 to look at associations between parental income until children are 15 and the risk of schizophrenia later in life for children.
Authors: Christian Hakulinen, Ph.D., of the University of Helsinki in Finland, is the corresponding author.
(doi:10.1001/jamapsychiatry.2019.2299)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
How Much Cardiovascular Disease Among Black Adults is Attributable to Hypertension?
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, OCTOBER 23, 2019
Media advisory: To contact corresponding author Donald Clark III, M.D., M.P.H., email Annie Oeth at aoeth@umc.edu. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2019.3773?guestAccessKey=9c5bc61e-ebca-4e25-8d88-ff077a402bdb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102319
Bottom Line: Estimating the proportion of cardiovascular disease (CVD) cases among black adults associated with hypertension was the focus of this observational study. The analysis included data on nearly 12,500 black adults in the United States, of whom 9,633 had hypertension. Researchers calculated population-attributable risk, which represents the proportion of cases of a disease in a population attributed to a risk factor. The findings suggest nearly one-third (32.5%) of CVD cases were associated with hypertension. Interventions to maintain normal blood pressure throughout life may help reduce CVD among black adults. A limitation of the study is that a common risk factor, such as hypertension, can make estimates of population-attributable risk less precise.
Authors: Donald Clark III, M.D., M.P.H., of the University of Mississippi Medical Center, Jackson, and coauthors.
(doi:10.1001/jamacardio.2019.3773)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
English Proficiency Associated With Hospital Revisits, Readmissions
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, OCTOBER 22, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.13066?guestAccessKey=776f620c-15cf-4df6-b98a-cb57bdc28a20&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102219
What The Study Did: Patients with limited English proficiency face barriers in health care settings. This observational study examined whether return emergency department visits or hospital readmissions differed between English-proficient patients and those with limited proficiency who were discharged with acute (pneumonia and hip fracture) and chronic (chronic obstructive pulmonary disease and heart failure) conditions from two Toronto hospitals.
Authors: Shail Rawal, M.D., M.P.H., of the University of Toronto, is the corresponding author.
(doi:10.1001/jama.2019.13066)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3804?guestAccessKey=28c20609-a669-4a04-9ee3-2af51c7a2551&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102119
Trial Compares SSRI vs. Placebo for Obsessive-Compulsive Behaviors in Kids, Teens With ASD
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, OCTOBER 22, 2019
Media advisory: To contact corresponding author Dinah S. Reddihough, M.D., email dinah.reddihough@rch.org.au. The full study and editorial are linked to this news release. A visual abstract is below.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.14685?guestAccessKey=51958aff-a578-4f40-8196-0293f4d957b7&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102219
Bottom Line: Researchers compared the selective serotonin reuptake inhibitor (SSRI) fluoxetine with placebo for reducing the frequency and severity of obsessive-compulsive behaviors in children and adolescents with autism spectrum disorder (ASD) in this randomized clinical trial in Australia. The trial included 146 participants (ages 7 to 18) with ASDs; 75 received fluoxetine and 71 received placebo for 16 weeks. Of the participants, 109 completed the trial. The authors report that for the primary outcome (total scores on an obsessive-compulsive scale modified for pervasive developmental disorder) treatment with fluoxetine compared with placebo resulted in lower scores for obsessive-compulsive behaviors but the interpretation of that finding is limited by a number of factors. These factors include the study’s high dropout rate and significant differences found between groups in some measures at baseline.
Authors: Dinah S. Reddihough, M.D., of the Royal Children’s Hospital, Melbourne, Australia, and coauthors.
(doi:10.1001/jama.2019.14685)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Clinical Trial in Japan Focuses on Avoiding Cow’s Milk Formula to Supplement Breastfeeding
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 21, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2019.3544?guestAccessKey=642cb0c8-a18e-4ee1-80bf-56994efc073c&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102119
What The Study Did: A randomized clinical trial in Japan with about 300 newborns looked at whether avoiding cow’s milk formula to supplement breastfeeding would decrease risks of sensitization to cow’s milk protein or food allergy, including cow’s milk allergy.
Author: Mitsuyoshi Urashima, M.D., M.P.H., Ph.D., of the Jikei University School of Medicine in Tokyo, is the corresponding author.
(doi:10.1001/jamapediatrics.2019.3544)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Analysis of US Pharmacy Closures
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 21, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.4588?guestAccessKey=9f0d3d86-193b-40b4-a8de-5d015f8842ab&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102119
What The Study Did: This research letter reports on pharmacy closures in the United States and risk factors associated with closure.
Authors: Dima M. Qato, Pharm.D., M.P.H., Ph.D., of the University of Illinois at Chicago, is the corresponding author.
(doi:10.1001/jamainternmed.2019.4588)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Is Cigarette Type Associated With Lung Cancer Outcomes?
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, OCTOBER 21, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article: This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2019.3487?guestAccessKey=40e559a5-e128-4289-b617-a70f476d7dee&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102119
What The Study Did: An association between lung cancer outcomes and the filter status of cigarettes, their tar level and menthol flavor was examined using data from more than 14,000 participants in a lung screening trial who completed detailed questionnaires about smoking.
Authors: Nichole T. Tanner, M.D., M.S.C.R., of the Ralph H. Johnson Veterans Affairs Hospital in Charleston, South Carolina, is the corresponding author.
(doi:10.1001/jamainternmed.2019.3487)
Editor’s Note: The article contains conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Born Premature, How Common to be Adult With No Major Health Conditions?
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, OCTOBER 22, 2019
Media advisory: To contact corresponding author Casey Crump, M.D., Ph.D., email Tildy La Farge at Tildy.lafarge@mountsinai.org. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.15040?guestAccessKey=001a2beb-213b-4149-92e0-b4d852bf2b94&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=102219
Bottom Line: This observational study looked at how common it was for people born premature to become adults without any major health conditions such as asthma, hypertension, diabetes and epilepsy, all of which have been associated with preterm birth. This analysis included birth registry data in Sweden for more than 2.5 million people born from 1973 to 1997, of whom 149,065 were born preterm (gestational age less than 37 weeks). Of all those born preterm, 54.6% were alive with no major medical conditions at ages 18 to 43 compared with 63% of people born at full-term. Limitations of the study include that detailed clinical data weren’t available to validate health conditions and longer follow-up is needed to examine outcomes after the age of 43.
Authors: Casey Crump, M.D., Ph.D., Icahn School of Medicine at Mount Sinai, New York, and coauthors.
(doi:10.1001/jama.2019.15040)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
New Video Accompanies Article About Waste in US Health Care System
JAMA
FOR IMMEDIATE RELEASE: Tuesday, October 15, 2019
Media advisory: To contact corresponding author William H. Shrank, M.D., M.S.H.S., email Alex Kepnes at akepnes@humana.com. The full study, editorials, summary video and podcast are linked to this news release. The video can be viewed on this page and embedded on your website by copying and pasting the HTML code below.
Embed this link to provide your readers free access to the full-text article https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2019.13978?guestAccessKey=bf8f9802-be69-4224-a67f-42bf2c53e027&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=100719
Bottom Line: A new study estimates about one-quarter of total health care spending in the United States is waste, with a price tag ranging from $760 billion to $935 billion. The United States spends more on health care than any other country. For this analysis, the authors identified government-based reports, articles and peer-reviewed publications from 2012 to 2019 that focused on estimates of costs or savings related to six areas of waste. There were 71 estimates from 54 publications and those estimates were combined into ranges or totaled. Study authors report total estimated annual cost of waste was $265.6 billion for administrative complexity (billing and coding waste, physician time spent reporting on quality measures); $230.7 billion to $240.5 billion for pricing failure (prices increase far from those expected in a well-functioning market); $102.4 billion to $165.7 billion for failure of care delivery (poor execution or lack of widespread adoption of best care processes); $75.7 billion to $101.2 billion for overtreatment or low-value care; $58.5 billion to $83.9 billion for fraud and abuse; and $27.2 billion to $78.2 billion for failure of care coordination (unnecessary admissions or avoidable complications and readmissions). The authors also searched the published literature to find estimates of the potential to reduce waste in each of the categories listed by scaling proven strategies. Projected potential savings from efforts to reduce waste ranged from $191 billion to $282 billion, a potential 25% reduction in the total cost of waste. The authors highlight the opportunity to reduce waste through insurer-clinician collaboration and data interoperability. This analysis has limitations, including that the studies used may not represent all costs and savings in each area of waste, and that data from some of the studies may not be generalizable to the U.S. population. Implementing effective measures to decrease waste is a chance to reduce continued increases in U.S. health care costs.
Authors: William H. Shrank, M.D., M.S.H.S., Humana Inc., Louisville, Kentucky, and coauthors
Video embed code:
(doi:10.1001/jama.2019.13978)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Aspirin Use After Biliary Tract Cancer Diagnosis
JAMA Oncology
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, OCTOBER 17, 2019
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2019.4328?guestAccessKey=4b431465-c9dc-4248-b994-80f4c972fac7&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=101719
What The Study Did: Researchers in this observational study examined if aspirin use after a diagnosis of a biliary tract cancer, which includes gallbladder cancer, was associated with reduced risk of death among nearly 3,000 patients.
Authors: Sarah S. Jackson, Ph.D., of the National Cancer Institute in Rockville, Maryland, is the corresponding author.
(doi:10.1001/jamaoncol.2019.4328)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Examining Depression, Postoperative Regret After Major Head/Neck Surgery
JAMA Otolaryngology-Head & Neck Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, OCTOBER 17, 2019
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/10.1001/jamaoto.2019.3020?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=101719
What The Study Did: Researchers investigated whether frail or elderly patients with head and neck cancer have worse depression or higher rates of regret after surgery.
Authors: David P. Goldstein, M.D., M.Sc., of the University of Toronto, is the corresponding author.
(doi:10.1001/jamaoto.2019.3020)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
