Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.0631?guestAccessKey=b073d126-e36d-4df9-a471-04f1b59ad3ba&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041520
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.0659?guestAccessKey=60132b4c-834c-4f4b-9224-b195f69eaee7&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041520
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.0527?guestAccessKey=c6eb127f-cf11-4af0-ba34-10f74797a55e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041520
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2791?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=041520
Suicide Mortality and COVID-19
JAMA Psychiatry
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 10, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.1060?guestAccessKey=c40eefb2-c634-47ed-b3c3-f00b005e3cf2&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041020
What The Viewpoint Says: Reasons why U.S. suicide rates may rise in tandem with the coronavirus disease 2019 (COVID-19) pandemic are explained in this article that also describes opportunities to expand research and care.
Authors: Mark A. Reger, Ph.D., of the VA Puget Sound Health Care System, and Seattle, Washington; and the University of Washington in Seattle, is the corresponding author.
(doi:10.1001/jamapsychiatry.2020.1060)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Working Together to Combat Mental Health Challenges During COVID-19 Pandemic
JAMA Psychiatry
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 10, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.1057?guestAccessKey=a92595b9-4663-4cff-a426-154c10ef69af&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041020
What The Viewpoint Says: This article offers lessons from Hubei, China, on potential methods to focus on mental health during the coronavirus disease 2019 (COVID-19) pandemic.
Authors: Yu-Tao Xiang, M.D., Ph.D., of the University of Macau in the Macao Special Administrative Region, China, is the corresponding author.
(doi:10.1001/jamapsychiatry.2020.1057)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Examining Associations Between Ages of Parents, Grandparents and Autism Risk in Children
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, APRIL 15, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2868?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=041520
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Older age for parents has been associated with autism spectrum disorders (ASDs) in children, however little is known about the association between the age of grandparents at the time of the birth of the parent and the risk of ASD in the grandchildren. This association was investigated in an observational study with the use of data from Danish national health registries that included three generations and 1.4 million children born from 1990 to 2013.
Authors: Zeyan Liew, Ph.D., M.P.H., of the Yale School of Public Health in New Haven, Connecticut, is the corresponding author.
(doi:10.1001/jamanetworkopen.2020.2868)
Editor’s Note: The article includes funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2787?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=041420
How Common is Racial/Ethnic Discrimination in US Surgical Residency Programs?
JAMA Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, APRIL 15, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2020.0260?guestAccessKey=12783497-ea02-47b5-aa43-29d92404002e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041520
What The Study Did: Surveys from nearly 7,000 resident surgeons were used to evaluate how common racial/ethnic discrimination is in U.S. general surgery programs and how it’s associated with burnout, thoughts of quitting and suicide.
Authors: Yue-Yung Hu, M.D., M.P.H., of the Feinberg School of Medicine at Northwestern University in Chicago, is the corresponding author.
(doi:10.1001/jamasurg.2020.0260)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Mental Health Consequences of COVID-19, Physical Distancing
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 10, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.1562?guestAccessKey=628c2154-eb34-4687-ae2f-651415708d7a&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041020
What The Viewpoint Says: The article emphasizes the importance of mitigating the mental health consequences of social distancing in the COVID-19 era.
Authors: Sandro Galea, M.D., of the Boston University School of Public Health, is the corresponding author.
(doi:10.1001/jamainternmed.2020.1562)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Neurologic Manifestations of Hospitalized Patients With COVID-19
JAMA Neurology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 10, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2020.1127?guestAccessKey=4acaca6e-7090-4008-acf2-54ded1321cfe&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041020
What The Study Did: This study investigates the neurologic symptoms of patients with coronavirus disease 2019 (COVID-19) in Wuhan, China.
Authors: Bo Hu, M.D., Ph.D., and Yanan Li, M.D., Ph.D., of Union Hospital, Tongji Medical College, Huazhong University of Science and Technology in Wuhan, China, are the corresponding authors.
(doi:10.1001/jamaneurol.2020.1127)
Editor’s Note: The article includes funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Is Birth by Cesarean Associated With Increased Risk of Obesity, Diabetes in Adulthood?
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 13, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2605?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=041320
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Risks for obesity and type 2 diabetes in adulthood were compared among 33,000 women born by cesarean or vaginal delivery between 1946 and 1964 in this observation study that included participants in the Nurses’ Health Study II.
Authors: Jorge E. Chavarro, M.D., Sc.D., of the Harvard T.H. Chan School of Public Health in Boston, is the corresponding author.
(doi:10.1001/jamanetworkopen.2020.2605)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Caring for Patients With Cancer Durring the COVID-19 Outbreak in Italy
JAMA Oncology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 10, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2020.1426?guestAccessKey=356c0b96-39e9-442b-9241-2e48eb781861&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041020
What The Article Says: An essay discusses the challenges associated with caring for patients with cancer during the COVID-19 epidemic in Italy.
Authors: Filippo Pietrantonio, M.D., and Marina Chiara Garassino, M.D., of the Fondazione IRCCS Istituto Nazionale dei Tumori in Milan, are the authors.
(doi:10.1001/jamaoncol.2020.1426)
Editor’s Note: The article includes conflict of interest disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Fertility Preservation Use Among Transgender Adolescents
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 13, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0264?guestAccessKey=72f4e88a-f7a0-437b-a9e4-3b96d595dda1&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041320
What The Study Did: Transgender adolescents often seek hormonal intervention to achieve a body consistent with their gender identity and those interventions affect reproductive function. This research letter examined the use of fertility preservation among transgender adolescents receiving hormonal intervention at a pediatric gender practice in Australia.
Authors: Kenneth C. Pang, M.B.B.S.(Hons), B.Med.Sc., Ph.D., of the Royal Children’s Hospital in Melbourne, Australia, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.0264)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Details of Treatment for Patients in China Who Died of COVID-19
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 10, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.5619?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=041020
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: This case series describes clinical characteristics of patients who died of coronavirus disease 2019 (COVID-19) in China.
Authors: Haibo Qiu, M.D., Ph.D., of Zhongda Hospital, Southeast University in Jiangsu, China, is the corresponding author.
(doi:10.1001/jamanetworkopen.2020.5619)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Potential Risks For Children Following Opioid-Related Overdose Death of a Parent
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 13, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0613?guestAccessKey=8bc52125-8033-4a27-81df-bf772299d55a&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041320
What The Study Did: Researchers examined changes in the use of mental health and human services among children in Allegheny County, Pennsylvania, following the unexpected death of a parent because of an opioid-related overdose between 2002 and 2017.
Authors: Eric G. Hulsey, Dr.P.H., M.A., of the Allegheny County Department of Human Services, Pittsburgh, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.0613)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Association of Blood Pressure Levels With Racial Differences in Cognitive Decline Risk
JAMA Neurology
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 13, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2020.0568?guestAccessKey=479ba9f0-cd89-4c1e-8bbc-d6a9d681b913&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041320
What The Study Did: This observational study pooled data from five study groups to examine whether cumulative blood pressure levels might explain racial differences in risk for cognitive decline later in life.
Authors: Deborah A. Levine, M.D., M.P.H., of the University of Michigan in Ann Arbor, is the corresponding author.
(doi:10.1001/jamaneurol.2020.0568)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Loss of Smell in Patient With COVID-19
JAMA Otolaryngology–Head & Neck Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, APRIL 8, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/10.1001/jamaoto.2020.0832?guestAccessKey=39c261ad-5393-4c12-a853-31a0ccfc123e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040820
What The Study Did: The case of a patient with coronavirus disease 2019 (COVID-19) whose main symptom was a loss of smell without nasal obstruction is reported in this article.
Authors: Michael Eliezer, M.D, of Lariboisière University Hospital in Paris, is the corresponding author.
(doi:10.1001/jamaoto.2020.0832)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Risk of Suicide, Homicide, Unintentional Firearm Deaths at Home
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 13, 2020
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.0806?guestAccessKey=546427c1-9b6a-43d3-b4ea-28f272b2f90e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=041320
What The Study Did: Personal protection is often cited as a reason for owning a firearm. Researchers in this study looked at 647 firearm deaths that occurred in homes in King County, Washington, from 2011 to 2018 and whether they were indicated as suicide, criminal homicide, self-defense homicide, unintentional or undetermined.
Authors: Elissa K. Butler, M.D., of the University of Washington in Seattle, is the corresponding author.
(doi:10.1001/jamainternmed.2020.0806)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
COVID-19 in Children in Spain
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, APRIL 8, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.1346?guestAccessKey=769fb77c-48f2-4ea3-b9e5-1b0913752c32&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040820
What The Study Did: Describes testing for and treatment of children with coronavirus disease 2019 (COVID-19) in Madrid.
Authors: Alfredo Tagarro, Ph.D., M.D., of the Hospital Infanta Sofía de San Sebastián de los Reyes in Madrid, Spain, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.1346)
Editor’s Note: The article includes conflict of interest disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1844?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040920
Marijuana Withdrawal Symptoms Among Regular Users Who Quit
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, APRIL 9, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2370?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040920
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: This study combined the results of 47 studies with 23,000 participants to estimate how common cannabis withdrawal syndrome (symptoms include irritability, nervousness or anxiety, depression and headache) is among individuals who stop regular use.
Authors: Anees Bahji, M.D., of Queen’s University in Kingston, Ontario, Canada, is the corresponding author.
(doi:10.1001/jamanetworkopen.2020.2370)
Editor’s Note: The article includes conflict of interest disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Firework-Related Eye Injuries
JAMA Ophthalmology
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, APRIL 9, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaophthalmology/fullarticle/10.1001/jamaophthalmol.2020.0832?guestAccessKey=a19033ae-c3d4-4dc1-90b4-03f4ab571eae&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040920
What The Study Did: Emergency department data were used to describe the number, type, severity and factors associated with firework-related eye injuries that occurred in the United States from 1999 to 2017.
Authors: Natasha Nayak Kolomeyer, M.D., of Thomas Jefferson University in Philadelphia, is the corresponding author.
(doi:10.1001/jamaophthalmol.2020.0832)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
What Other Countries Can Learn From Italy During the COVID-19 Pandemic
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, APRIL 7, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.1447?guestAccessKey=c520cc85-bd2e-4ba0-8f99-ac75c8b5ef25&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040720
What The Viewpoint Says: Exploring the challenges in the Italian health care system during the coronavirus disease 2019 pandemic and how other countries can plan for optimal actions.
(doi:10.1001/jamainternmed.2020.1447)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
US Public Concerns About COVID-19 Pandemic
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, APRIL 7, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.1369?guestAccessKey=cd7f419d-b177-44d2-86b2-c3e0254b3152&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040720
What The Study Did: This survey study assessed public concerns about symptoms of coronavirus disease 2019 and individual actions in response to the pandemic.
(doi:10.1001/jamainternmed.2020.1369)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Electronic Cigarette Use Among Young Adult Cancer Survivors
JAMA Oncology
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, APRIL 9, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2020.0384?guestAccessKey=866f0b23-ca71-4e00-bb0c-83c3de82d510&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040920
What The Study Did: This study used national survey data from young adults ages 18 to 39 to compare e-cigarette use among cancer survivors with their peers without cancer.
Authors: Helen M. Parsons, Ph.D., M.P.H., of the University of Minnesota in Minneapolis, is the corresponding author.
(doi:10.1001/jamaoncol.2020.0384)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2306?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040820
Examining Association of Preoperative Metformin, Surgical Outcomes in Patients With Diabetes
JAMA Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, APRIL 8, 2020
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2020.0416?guestAccessKey=e4c484c5-2f05-4eaf-810c-de47feb2e76e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040820
What The Study Did: Metformin is the most commonly prescribed noninsulin medication for type 2 diabetes and this observational study examined postoperative death and hospital readmission among adults with type 2 diabetes who had a prescription for metformin before major surgery with those who didn’t.
Authors: Christopher W. Seymour, M.D., M.Sc., of the Clinical Research, Investigation and Systems Modeling of Acute Illness Center in Pittsburgh, is the corresponding author.
(doi:10.1001/jamasurg.2020.0416)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Differences by Race/Ethnicity in Stage at Diagnosis, Treatment, Survival for Cancers
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, APRIL 8, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2950?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040820
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Data for 950,000 black, white, Asian and Hispanic patients in the U.S. diagnosed with prostate, ovarian, breast, stomach, pancreatic, lung, liver, esophageal, or colorectal cancers were analyzed to examine differences by race and ethnicity in stage at diagnosis, use of therapy, overall survival and cancer-specific survival.
Authors: Haiyong Wang, Ph.D., of the Shandong First Medical University and Shandong Academy of Medical Sciences in Shandong, China, is the corresponding author.
(doi:10.1001/jamanetworkopen.2020.2950)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.0316?guestAccessKey=b4f5495b-c03e-4998-a68f-1c661c2124d7&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040820
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Investigating Association Between Preconception Exposure to Plastics, Risk of Preterm Birth
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, APRIL 7, 2020
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2159?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040720
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Researchers used urinary measures of biomarkers of phthalates (a group of chemicals used in plastics) and phthalate substitutes from couples undergoing fertility care and examined if higher concentrations prior to conception were associated with an increased risk of preterm birth.
Authors: Carmen Messerlian, Ph.D., of the Harvard T.H. Chan School of Public Health in Boston, is the corresponding author.
(doi:10.1001/jamanetworkopen.2020.2159)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2187?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040620
COVID-19 Infection and Renin Angiotensin System Blockers
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 3, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.1282?guestAccessKey=e7664282-d295-4d2f-9c47-dc723f53ac67&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040320
What The Viewpoint Says: Discussion of recommendations for angiotensin-converting enzyme inhibitor and angiotensin receptor blocker use in patients with or at risk of contracting coronavirus disease 2019 (COVID-19).
Authors: Franz H. Messerli, M.D., of Bern University Hospital in Switzerland, is the corresponding author.
(doi:10.1001/jamacardio.2020.1282)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Dilemma of COVID-19, Aging and Cardiovascular Disease
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 3, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.1329?guestAccessKey=5ddaab2f-e4a3-4e1b-9b69-c523df1ab830&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040320
What The Viewpoint Says: Whether individuals should continue to take angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in the context of coronavirus disease 2019 (COVID-19) is discussed in this article.
Authors: Majd AlGhatrif, M.D., M.A., of the National Institutes of Health in Baltimore, is the corresponding author.
(doi:10.1001/jamacardio.2020.1329)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
What Pediatric Health Care Clinicians Need to Know
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, APRIL 3, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.1224?guestAccessKey=3052e8d2-712f-49d3-b4ef-c2fbab784fdc&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040320
What The Viewpoint Says: Information on the coronavirus disease 2019 pandemic that is useful for pediatric clinicians is in this article.
Authors: Sonja A. Rasmussen, M.D., M.S., of the University of Florida College of Medicine in Gainesville, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.1224)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2020.1943?guestAccessKey=8aa79439-281a-4e85-b689-efd02a874c9e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040720
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0208?guestAccessKey=b60c9bca-2c3b-4611-ac4b-7c624cb05a87&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040620
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.0681?guestAccessKey=1ee61837-fa7b-40dc-af59-07efccd82ad0&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040620
Examining Association Between Childhood Video Game Use, Adolescent Body Weight
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 6, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0202?guestAccessKey=45d70a5f-5902-467c-a6e5-b0fb936334c4&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040620
What The Study Did: Researchers looked at whether there was a long-term association between using video games at an early age and later weight as a teenager, as well as what role behaviors such as physical activity, the regularity of bedtimes and consuming sugar-sweetened beverages might play. The study was a secondary analysis of data from a study that included 16,000 children born in the United Kingdom.
Authors: Rebecca J. Beeken, Ph.D., of the University of Leeds in Leeds, England, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.0202)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Changes in Marijuana Vaping, Edible Use Among US 12th Graders
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 6, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0175?guestAccessKey=51755167-693f-405e-9060-3668f5c1ed15&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040620
What The Study Did: About 2,400 students in the 12th grade were surveyed about the frequency and mode of use (smoking, vaping and edibles) of marijuana from 2015 to 2018.
Authors: Megan E. Patrick, Ph.D., of the University of Minnesota in Minneapolis, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.0175)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Which Healthy Lifestyle Factors Associated With More Years Free of Chronic Disease?
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, APRIL 6, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.0618?guestAccessKey=a2e886d8-1d4c-423f-9928-4ec9535010b4&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040620
What The Study Did: What combination of healthy lifestyle factors were associated with the most years lived without chronic diseases was the focus of this analysis that included data from more than 100,000 adults who were participants in 12 European studies. Participants’ levels of smoking, weight, physical activity and alcohol consumption were compared with the number of years from age 40 to 75 that they were without chronic disease, including type 2 diabetes, coronary heart disease, stroke, cancer, asthma and chronic obstructive pulmonary disease.
Authors: Solja T. Nyberg, Ph.D., of the University of Helsinki, is the corresponding author.
(doi:10.1001/jamainternmed.2020.0618)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2044?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040320
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2027?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040320
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2064?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040320
USPSTF Recommendation on Screening for Bacterial Vaginosis in Pregnancy
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, APRIL 7, 2020
Media advisory: To contact the U.S. Preventive Services Task Force, email the Media Coordinator at Newsroom@USPSTF.net or call 202-572-2044. The full report and related articles are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time and all USPSTF articles remain free indefinitely https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2020.2684?guestAccessKey=65882581-0679-4db4-895b-7179f28cdca5&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040720
Bottom Line: The U.S. Preventive Services Task Force (USPSTF) recommends against screening for bacterial vaginosis in someone without symptoms and who is pregnant but not at increased risk for preterm delivery. Bacterial vaginosis is a common condition caused by an overgrowth of bacteria in the vagina and it has been associated with adverse pregnancy outcomes including preterm delivery. The USPSTF found insufficient evidence to make a recommendation on screening those who are pregnant and at increased risk for preterm delivery. The USPSTF routinely makes recommendations about the effectiveness of preventive care services and this statement reaffirms its 2008 recommendations.
(doi:10.1001/jama.2020.2684)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Note: More information about the U.S. Preventive Services Task Force, its process, and its recommendations can be found on the newsroom page of its website.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email mediarelations@jamanetwork.org.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.2012?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040220
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1997?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=040220
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2020.0421?guestAccessKey=996ca4ae-c233-405e-bbb5-322b8a6f8c71&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040220
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaophthalmology/fullarticle/10.1001/jamaophthalmol.2020.0673?guestAccessKey=979ee77a-b8be-478a-94b7-da8a762d2be5&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040220
Ocular Findings of Patients With COVID-19
JAMA Ophthalmology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, MARCH 31, 2020
Media advisory: The full study and commentary are linked to this news release
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaophthalmology/fullarticle/10.1001/jamaophthalmol.2020.1291?guestAccessKey=6b204664-6c20-473d-9396-807bfb3ce7a8&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032120
What The Study Did: One-third of COVID-19 patients from Hubei, China, had ocular manifestations, occurring frequently in patients with more severe physical conditions.
Authors: Liang Liang, M.D., of China Three Gorges University in Yichang, China, and Kaili Wu, M.D., of Sun Yat-sen University Guangzhou, China, are the corresponding authors.
(doi:10.1001/jamaophthalmol.2020.1291)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Perspectives on COVID-19 Control Measures for Ophthalmology Clinics
JAMA Ophthalmology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, MARCH 31, 2020
Media advisory: The article is linked to this news release
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaophthalmology/fullarticle/10.1001/jamaophthalmol.2020.1288?guestAccessKey=cfd3ac72-e954-47d8-b81b-c40f03672f57&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=033120
What The Viewpoint Says: This article describes treatment initiatives being undertaken for novel coronavirus 2019 at an ophthalmology center in Singapore.
Authors: Ivan Seah Yu Jun, M.B.B.S., of National University Hospital of Singapore, is the corresponding author.
(doi:10.1001/jamaophthalmol.2020.1288)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Measures for Care of Cancer Patients During COVID-19 Outbreak in China
JAMA Oncology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, APRIL 1, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2020.1198?guestAccessKey=9dad6790-0e1e-41c8-92a3-65ea2ce138c4&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040120
What The Viewpoint Says: The authors describe measures taken to reduce the risk of transmitting severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) to medical staff and cancer patients seeking treatment during the COVID-19 outbreak in China.
Authors: Jie Wang, M.D., Ph.D., and Jie He, M.D., of the Chinese Academy of Medical Sciences & Peking Union Medical College in Beijing, are the corresponding authors.
(doi:10.1001/jamaoncol.2020.1198)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Safety Recommendations for Health Care Workers Involved With Head, Neck Exams, Surgery During COVID-19 Pandemic
JAMA Otolaryngology–Head & Neck Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, MARCH 31, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/10.1001/jamaoto.2020.0780?guestAccessKey=db0bf318-5be8-4871-be74-96595f84a832&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=033120
What The Study Did: Health care workers who come in close contact with a patient’s head and neck are particularly at risk for developing coronavirus disease 2019 (COVID-19) because of the rapid spread of severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2) through respiratory droplets. This article provides safety recommendations for these health care workers regarding exams and surgical procedures based on a review of the literature and the experiences of physicians with firsthand knowledge of safety procedures during this pandemic.
Authors: Babak Givi, M.D., of NYU Langone Health in New York, is the corresponding author.
(doi:10.1001/jamaoto.2020.0780)
Editor’s Note: The article includes conflict of interest disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamasurgery/fullarticle/10.1001/jamasurg.2020.0263?guestAccessKey=b9697936-a7c3-4fe7-8614-4a47c9f0255c&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040120
Surgical Considerations for Tracheostomy During COVID-19 Pandemic
JAMA Otolaryngology–Head & Neck Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, MARCH 31, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/10.1001/jamaoto.2020.0764?guestAccessKey=7f332b4b-6ee2-4fdd-8e72-2daf267abd47&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=033120
What The Viewpoint Says: Lessons learned from the 2003 severe acute respiratory syndrome (SARS) epidemic may help reduce the spread of severe acute respiratory syndrome coronavirus 2 (SARS- CoV-2), the cause of coronavirus disease 2019 (COVID-19), to health care workers performing open tracheostomies, a surgical procedure to open an airway that may be required for many patients with COVID-19.
Authors: Woei Shyang Loh, M.B.B.S., of the National University of Singapore, is the corresponding author.
(doi:10.1001/jamaoto.2020.0764)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.0322?guestAccessKey=d1c41ee8-805d-411e-bc3e-80dd1365cb08&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040120
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.0306?guestAccessKey=720b34b3-d3a5-4450-a68e-ef9fee996b22&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=040120
Cardiovascular Implications of Fatal Outcomes of Patients With COVID-19
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, MARCH 27, 2020
Media advisory: The full article and editor are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.1017?guestAccessKey=bb0c7e82-f99b-40d1-a5f6-ad104814b539&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032720
What The Study Did: Evaluating the association of underlying cardiovascular disease and myocardial injury on fatal outcomes in patients with coronavirus disease 2019 (COVID-19).
Authors: Zhibing Lu, M.D., and Xinghuan Wang, M.D., of Zhongnan Hospital of Wuhan University in China, are the corresponding authors.
(doi:10.1001/jamacardio.2020.1017)
Editor’s Note: The article includes funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Cardiac Involvement in a Patient With COVID-19
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, MARCH 27, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.1096?guestAccessKey=a87f2a9c-ef04-4f19-b396-c6ff6568d51d&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032720
What The Study Did: A description of the presentation of acute myocardial inflammation in a patient with coronavirus disease 2019 (COVID-19) who recovered from influenzalike syndrome and developed fatigue and signs and symptoms of heart failure a week after upper respiratory tract symptoms.
Authors: Marco Metra, M.D., of the Institute of Cardiology in Brescia, Italy, is the corresponding author.
(doi:10.1001/jamacardio.2020.1096)
Editor’s Note: The article includes conflict of interest disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Potential Effects of Coronaviruses on the Cardiovascular System
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, MARCH 27, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.1286?guestAccessKey=150724fb-8146-4fc2-a60c-b78955728d41&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032720
What The Study Did: An overview of the basics of coronaviruses, with a focus on coronavirus disease 2019 (COVID-19) along with their effects on the cardiovascular system.
Authors: Mohammad Madjid, M.D., M.S., of the University of Texas Health Science Center at Houston, is the corresponding author.
(doi:10.1001/jamacardio.2020.1286)
Editor’s Note: Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Investigating SARS-CoV-2 Transmission in Public Bath Center in China
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 30, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.4583?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=033020
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: This case series reports a cluster-spreading event in Huai’an (about 435 miles northeast of Wuhan) in Jiangsu Province, China, where a patient with SARS-CoV-2 may have transmitted the virus to eight other healthy individuals through bathing in a public bath center.
Authors: Qilong Wang, M.D., Ph.D., of the Affiliated Huai’an No. 1 People’s Hospital, Nanjing Medical University in Huai’an, China, and Hongbing Shen, M.D., Ph.D., of the School of Public Health, Nanjing Medical University in Nanjing, China, are the corresponding authors.
(10.1001/jamanetworkopen.2020.4583)
Editor’s Note: The article includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0129?guestAccessKey=a0ac719c-5c67-4f08-95fa-10e252fb1cf4&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=033020
Investigating Association Between Air Pollution, Dementia Risk and Role of Cardiovascular Disease
JAMA Neurology
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 30, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2019.4914?guestAccessKey=9b6ee148-fb0a-42f9-a5fb-183c2a41342d&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=033020
What The Study Did: This observational study analyzed data from about 2,900 older residents of Stockholm to examine the association between long-term exposure to air pollution and the risk of developing dementia, along with what role cardiovascular disease might have.
Authors: Giulia Grande, M.D., of the Karolinska Institutet and Stockholm University in Stockholm, is the corresponding author.
(doi:10.1001/jamaneurol.2019.4914)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Infants Born to Mothers With COVID-19 in China
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, MARCH 26, 2020
Media Advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0878?guestAccessKey=39d64ff4-cadb-4cbf-a8af-a36401f80ccb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032620
What The Study Did: This study examined the medical records of 33 newborns born to women with COVID-19.
Author: Wenhao Zhou, M.D., of the National Children’s Medical Center, Children’s Hospital of Fudan University in Shanghai, China, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.0878)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaophthalmology/fullarticle/10.1001/jamaophthalmol.2020.0531?guestAccessKey=6a6011b5-2a74-4ad6-a0b4-14d042680fc6&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032620
SARS-CoV-2 Transmission in Patients With Cancer at a Hospital in China
JAMA Oncology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, MARCH 25, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2020.0980?guestAccessKey=958b15ee-5658-4cbf-9d3d-f7a1639c4f5a&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032520
What The Study Did: Researchers estimated the infection rate of SARS-CoV-2 in patients with cancer and reported on patient outcomes at a single hospital in Wuhan, China.
Authors: Conghua Xie, M.D., of Zhongnan Hospital of Wuhan University in China, and Melvin L. K. Chua, M.B.B.S., Ph.D., of the National Cancer Centre Singapore, are the corresponding authors.
(doi:10.1001/jamaoncol.2020.0980)
Editor’s Note: The article includes funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
estimated the infection rate of SARS-CoV-2 in pa- tients with cancer and report on patient outcomes from a single hospital in Wuhan, China.
Investigating Spaceflight-Associated Changes in Astronauts
JAMA Otolaryngology–Head & Neck Surgery
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, MARCH 26, 2020
Media advisory: The full study and commentary is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/10.1001/jamaoto.2020.0228?guestAccessKey=ab4ab54b-38e8-4ebd-83c6-f82fff482d8f&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032620
What The Study Did: Head congestion is one of the most common symptoms experienced by astronauts during spaceflight. This observational study examined preflight and postflight head magnetic resonance images (MRIs) of 35 astronauts who participated in either a short-duration (30 days or less) Space Shuttle mission or a long-duration (greater than 30 days) International Space Station mission. Researchers investigated whether there were differences in the development of certain physiological changes of the paranasal sinuses and mastoid air cells associated with symptoms of head congestion.
Authors: Donna R. Roberts, M.D., of the Medical University of South Carolina in Charleston, is the corresponding author.
(doi:10.1001/jamaoto.2020.0228)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Observation vs. Targeted High-Dose Radiation for Metastatic Prostate Cancer
JAMA Oncology
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, MARCH 26, 2020
Media advisory: The full study and commentary are linked to this news release. A visual abstract is below.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaoncology/fullarticle/10.1001/jamaoncol.2020.0147?guestAccessKey=e5501192-c562-4e38-9167-81da44e28982&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032620
What The Study Did: This randomized clinical trial compared how effectively high-dose, targeted radiation therapy versus no treatment (observation) among 54 men prevented the progression over six months of recurrent hormone-sensitive prostate cancer that has metastasized to a small number of sites in the body.
Authors: Phuoc T. Tran, M.D., Ph.D., of the Johns Hopkins University School of Medicine in Baltimore, is the corresponding author.
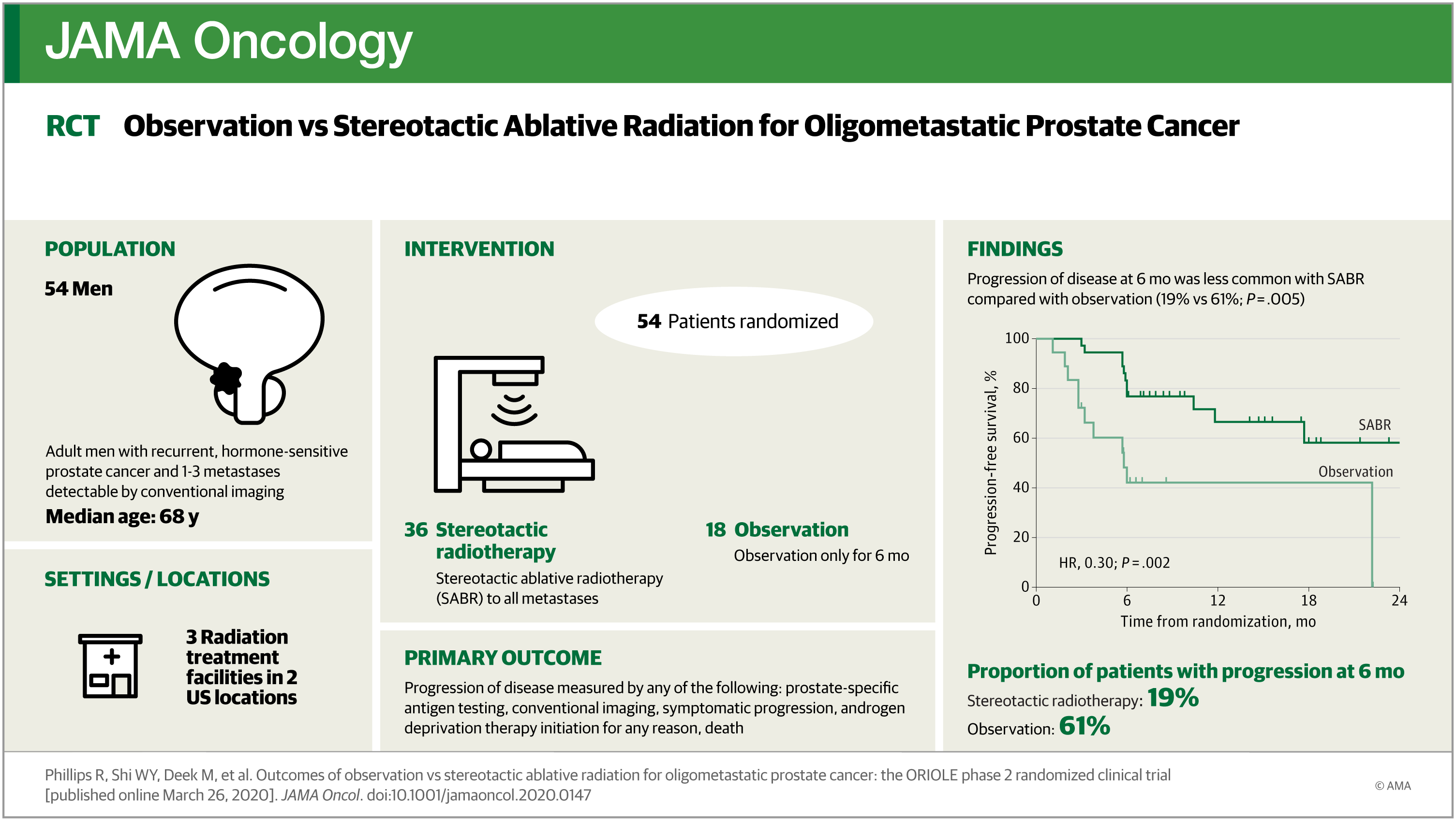
(doi:10.1001/jamaoncol.2020.0147)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
An Acute Respiratory Infection Runs Into the Most Common Noncommunicable Epidemic— COVID-19 and Cardiovascular Diseases
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, MARCH 25, 2020
Media advisory: The full article is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.0934?guestAccessKey=77602fbc-4085-4c24-a891-1f2e1daf3d80&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032520
What The Viewpoint Says: Emerging as an acute infectious disease, COVID-19 may be- come a chronic epidemic similar to influenza because of genetic re- combination. Therefore, we should be ready for the reemergence of COVID-19 or other coronaviruses.
(doi:10.1001/jamacardio.2020.0934)
Editor’s Note: The article includes funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations..
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamadermatology/fullarticle/10.1001/jamadermatol.2020.0480?guestAccessKey=ee5d32a9-728a-496e-9a21-862aab5f9d90&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032520
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamadermatology/fullarticle/10.1001/jamadermatol.2020.0470?guestAccessKey=c13e6072-caf7-4212-845e-5826ac19368f&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032520
Association of Cardiac Injury With Mortality in Hospitalized Patients With COVID-19 in Wuhan, China
JAMA Cardiology
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, MARCH 25, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamacardiology/fullarticle/10.1001/jamacardio.2020.0950?guestAccessKey=f0e95b50-fbb4-4d35-9306-e55e01f820bd&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032520
What The Study Did: This observational study of 416 patients in Wuhan, China, with confirmed coronavirus disease 2019 (COVID-19) reports that cardiac injury is a common condition among hospitalized patients with COVID-19 and it is associated with higher risk of in-hospital mortality.
Authors: Bo Yang, M.D., Ph.D., and He Huang, M.D., Ph.D., of Renmin Hospital of Wuhan University in China, are the corresponding authors.
(doi:10.1001/jamacardio.2020.0950)
Editor’s Note: The article includes funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Cardiac injury is a common condition among hospitalized patients with COVID-19 in Wuhan, China, and it is associated with higher risk of in-hospital mortality.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.0217?guestAccessKey=1003bdfc-a427-4ad1-968d-cf1fe985707e&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032520
Mental Health Care for Adolescents
JAMA Psychiatry
EMBARGOED FOR RELEASE: 11 A.M. (ET), WEDNESDAY, MARCH 25, 2020
Media advisory: To contact corresponding author Ramin Mojtabai, M.D., Ph.D., M.P.H., email Barbara Benham at bbenham1@jhu.edu. The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapsychiatry/fullarticle/10.1001/jamapsychiatry.2020.0279?guestAccessKey=0b773dd8-19b9-4aec-b2df-a6cb35b24827&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032520
What The Study Did: Researchers examined changes over time in the kinds of mental health problems for which adolescents in the United States received care and where they got that care in this survey study with findings that should be interpreted within the context of several limitations including self-reported information.
Authors: Ramin Mojtabai, M.D., Ph.D., M.P.H., of the Johns Hopkins Bloomberg School of Public Health in Baltimore, is the corresponding author.
(10.1001/jamapsychiatry.2020.0279)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1417?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032420
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1511?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032420
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0028?guestAccessKey=f8ad6f95-8ddd-4608-807b-e9dd97d371d0&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0002?guestAccessKey=e74b47fd-24d2-4cc5-9775-acd172e9ebeb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0052?guestAccessKey=0424c958-e7b7-408b-9cce-922bf8afe7a5&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0085?guestAccessKey=77191b31-fa42-4b6e-b257-18bbbd689c5c&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.0607?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032320
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1600?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032320
Mental Health of Health Care Workers in China in Hospitals With Patients With COVID-19
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 23, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.3976?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032320
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: This survey study of almost 1,300 health care workers in China at 34 hospitals equipped with fever clinics or wards for patients with COVID-19 reports on their mental health outcomes, including symptoms of depression, anxiety, insomnia and distress.
Authors: Zhongchun Liu, M.D., of the Renmin Hospital of Wuhan University, in Wuhan, and Shaohua Hu, M.D., of the First Affiliated Hospital, Zhejiang University School of Medicine in Hangzhou, China, are the corresponding authors.
(10.1001/jamanetworkopen.2020.3976)
Editor’s Note: The study includes funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Associations Between Screen Use, Language Skills
JAMA Pediatrics
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 23, 2020
Media Advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamapediatrics/fullarticle/10.1001/jamapediatrics.2020.0327?guestAccessKey=ac46b108-a6b5-4eb1-9b18-f18095433f71&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
What The Study Did: Researchers combined the results of 42 studies in this analysis to examine associations between the quantity, quality and onset of screen use by children and language skills.
Author: Sheri Madigan, Ph.D., of the University of Calgary in Canada, is the corresponding author.
(doi:10.1001/jamapediatrics.2020.0327)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2020.0542?guestAccessKey=8610f237-e477-4933-a9f2-f1f21d1313a2&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032420
Study Examines Association of Sleep-Disordered Breathing With Alzheimer Disease Biomarkers
JAMA Neurology
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 23, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaneurology/fullarticle/10.1001/jamaneurol.2020.0311?guestAccessKey=fdbc1d49-7abc-434f-9309-9983b8a38ca5&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
What The Study Did: This study used data and brain imaging from a randomized clinical trial for older adults who are cognitively unimpaired and examined brain changes, including the presence of biomarkers for Alzheimer disease, between those with sleep-disordered breathing and those without.
Authors: Gael Chetelat, Ph.D., of the Universite de Caen in France, is the corresponding author.
(doi:10.1001/jamaneurol.2020.0311)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Estimating Breast Cancer Screening Use, Costs Among Women in 40s With Private Insurance
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 23, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.0262?guestAccessKey=960a34b5-c0a5-4f44-83f0-b3c18ffd9fef&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
What The Study Did: Researchers used a large commercial claims database to estimate the percentage of U.S. women in their 40s with private insurance who were eligible and received screening mammography in 2017 and national costs for this screening.
Authors: Natalia Kunst, M.Sc., of the University of Oslo in Norway, is the corresponding author.
(doi:10.1001/jamainternmed.2020.0262)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1396?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032020
Examining Racial Disparities in Prostate Cancer Survival
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, MARCH 31, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1839?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=033120
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Data for nearly 230,000 men were used in this study to examine variations in survival in prostate cancer by geographic areas in the United States.
Authors: Quoc-Dien Trinh, M.D., of Harvard Medical School and Brigham and Women’s Hospital in Boston, is the corresponding author.
(10.1001/jamanetworkopen.2020.1839)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Study Compares Funding, Research Productivity for 2 Diseases
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, MARCH 27, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1737?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032720
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: This study compared federal and foundation research funding for sickle cell disease and cystic fibrosis and investigated whether funding was associated with differences in drug development and research productivity.
Authors: John J. Strouse, M.D., Ph.D., of Duke University School of Medicine in Durham, North Carolina, is the corresponding author.
(10.1001/jamanetworkopen.2020.1737)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Comparing Opioid-Related Emergency Department Visits, Hospitalizations Before, After ACA Medicaid Expansion
JAMA Internal Medicine
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 23, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/10.1001/jamainternmed.2020.0473?guestAccessKey=cba791ff-d9f8-430f-9a35-ae477bae83eb&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032320
What The Study Did: This observational study compared changes in opioid-related emergency department visits and hospitalizations before and after the 2014 Affordable Care Act (ACA) Medicaid expansion in states that implemented expansions with states that didn’t. Medicaid expansions improve access to outpatient treatment and have the potential to reduce opioid-related hospital use.
Authors: Aparna Soni, Ph.D., of American University in Washington, D.C., is the corresponding author.
(doi:10.1001/jamainternmed.2020.0473)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Overdose Risk Among Youth With Family Members Prescribed Opioids
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), FRIDAY, MARCH 27, 2020
Media advisory: The full study and commentary are linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1018?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032720
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: In this study of 72,000 adolescents and young adults, higher risk of youth overdose was associated with exposure to family members with opioid prescriptions and young people’s own opioid prescriptions.
Authors: Anh P. Nguyen, Ph.D., of the Institute for Health Research, Kaiser Permanente Colorado, is the corresponding author.
(10.1001/jamanetworkopen.2020.1018)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Injuries From Motorized Scooters
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, MARCH 31, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1925?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=033120
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Motorized scooters are increasingly popular and, in this study, researchers analyzed medical information for 61 adults who visited a single emergency department with scooter-related injuries.
Authors: Jeffrey D. Riley, M.D., of HonorHealth Scottsdale Osborn Medical Center in Arizona, is the corresponding author.
(10.1001/jamanetworkopen.2020.1925)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Comparing Recall Rates, Cancer Detection in Breast Cancer Screenings
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), MONDAY, MARCH 30, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1759?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=033020
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Nearly 200 radiologists who interpreted about 251,000 digital breast tomosynthesis (DBT) and 2 million digital mammography screening examinations were included in this observational study that evaluated recall and cancer detection rates.
Authors: Brian L. Sprague, Ph.D., of the University of Vermont in Burlington, is the corresponding author.
(10.1001/jamanetworkopen.2020.1759)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Depression Severity, Care Among Older Adults From Different Racial/Ethnic Groups
JAMA Network Open
EMBARGOED FOR RELEASE: 11 A.M. (ET), THURSDAY, MARCH 26, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2020.1606?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=032620
About JAMA Network Open: JAMA Network Open is the new online-only open access general medical journal from the JAMA Network. On weekdays, the journal publishes peer-reviewed clinical research and commentary in more than 40 medical and health subject areas. Every article is free online from the day of publication.
What The Study Did: Racial and ethnic differences appear to exist in depression severity and care in this observational study of older adults who participated in a randomized clinical trial of cancer and cardiovascular disease prevention.
Authors: Olivia I. Okereke, M.D., S.M., of Massachusetts General Hospital in Boston, is the corresponding author.
(10.1001/jamanetworkopen.2020.1606)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the article for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Diet Quality of Young People in US
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, MARCH 24, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2020.0878?guestAccessKey=c034a323-4646-4d89-8724-d9c934a78df1&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032420
What The Study Did: This observational study used national survey data from young people up to age 19 to estimate the overall diet quality of children and teens in the United States and to explore how diet quality has changed from 1999 to 2016.
Authors: Junxiu Liu, Ph.D., of Tufts University in Boston, is the corresponding author.
(doi:10.1001/jama.2020.0878)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamaophthalmology/fullarticle/10.1001/jamaophthalmol.2020.0392?guestAccessKey=a6468937-bdb1-43eb-b603-3267fab82ad5&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=031920
Is Step Count Associated With Lower Risk of Death?
JAMA
EMBARGOED FOR RELEASE: 11 A.M. (ET), TUESDAY, MARCH 24, 2020
Media advisory: The full study is linked to this news release.
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2020.1382?guestAccessKey=9f6744af-eb6c-4e03-9bca-d85492e1acab&utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_content=tfl&utm_term=032420
What The Study Did: Researchers looked at whether taking more steps and higher intensity stepping were associated with reduced risk of death in this observational study that included almost 4,900 adults (40 and over) who wore a device called an accelerometer to measure their step count and step intensity (steps/minute).
Authors: Pedro F. Saint-Maurice, Ph.D., of the National Cancer Institute in Rockville, Maryland, is the corresponding author.
(doi:10.1001/jama.2020.1382)
Editor’s Note: The article includes conflict of interest and funding/support disclosures. Please see the articles for additional information, including other authors, author contributions and affiliations, conflicts of interest and financial disclosures, and funding and support.
# # #
For more information, contact JAMA Network Media Relations at 312-464-JAMA (5262) or email media relations.
Here’s a link to provide your readers free access to the full-text article
Embed this link to provide your readers free access to the full-text article This link will be live at the embargo time https://jamanetwork.com/journals/jamanetworkopen/fullarticle/10.1001/jamanetworkopen.2019.19713?utm_source=For_The_Media&utm_medium=referral&utm_campaign=ftm_links&utm_term=031920
