EMBARGOED FOR RELEASE: 11 A.M. (ET) TUESDAY, DECEMBER 20, 2016
Media Advisory: To contact the U.S. Preventive Services Task Force, email the Media Coordinator at Newsroom@USPSTF.net or call 202-572-2044.
To place an electronic embedded link to this report in your story This link will be live at the embargo time: https://jamanetwork.com/journals/jama/fullarticle/10.1001/jama.2016.16776
JAMA
The U.S. Preventive Services Task Force (USPSTF) recommends against routine serologic screening (via a blood test) for genital herpes simplex virus infection in asymptomatic adolescents and adults, including those who are pregnant. The report appears in the December 20 issue of JAMA.
This is a D recommendation, indicating that there is moderate or high certainty that the screening has no net benefit or that the harms outweigh the benefits.
Genital herpes is a prevalent sexually transmitted infection in the United States; the Centers for Disease Control and Prevention estimates that almost 1 in 6 persons ages 14 to 49 years have genital herpes. Genital herpes infection is caused by 2 subtypes of herpes simplex virus (HSV), HSV-1 and HSV-2. Unlike other infections for which screening is recommended, HSV infection may not have a long asymptomatic period during which screening, early identification, and treatment may alter its course. Antiviral medications may provide symptomatic relief from outbreaks; however, these medications do not cure HSV infection. Although transmission of HSV can occur between an infected pregnant woman and her infant during vaginal delivery, interventions can help reduce transmission.
To update its 2005 recommendation on screening for genital herpes, the USPSTF reviewed the evidence on the accuracy, benefits, and harms of serologic screening for HSV-2 infection in asymptomatic persons, including those who are pregnant, as well as the effectiveness and harms of preventive medications and behavioral counseling interventions to reduce future symptomatic episodes and transmission to others.
The USPSTF is an independent, volunteer panel of experts that makes recommendations about the effectiveness of specific preventive care services such as screenings, counseling services, and preventive medications.
Detection
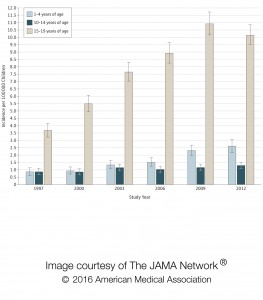
In the past, most cases of genital herpes in the United States have been caused by infection with HSV-2. Adequate evidence suggests that the most widely used, currently available serologic screening test for HSV-2 approved by the U.S. Food and Drug Administration is not suitable for population-based screening, based on its low specificity, the lack of widely available confirmatory testing, and its high false-positive rate. Rates of genital herpes due to HSV-1 infection in the United States may be increasing. While HSV-1 infection can be identified by serologic tests, the tests cannot determine if the site of infection is oral or genital; thus, these serologic tests are not useful for screening for asymptomatic genital herpes resulting from HSV-1 infection.
Benefits of Early Detection and Intervention
Based on limited evidence from a small number of trials on the potential benefit of screening and interventions in asymptomatic populations and an understanding of the natural history and epidemiology of genital HSV infection, the USPSTF concluded that the evidence is adequate to bound the potential benefits of screening in asymptomatic adolescents and adults, including those who are pregnant, as no greater than small.
Harms of Early Detection and Intervention
Based on evidence on potential harms from a small number of trials, the high false-positive rate of the screening tests, and the potential anxiety and disruption of personal relationships related to diagnosis, the USPSTF found that the evidence is adequate to bound the potential harms of screening in asymptomatic adolescents and adults, including those who are pregnant, as at least moderate.
Summary
Based on the natural history of HSV infection, its epidemiology, and the available evidence on the accuracy of serologic screening tests, the USPSTF concluded that the harms outweigh the benefits of serologic screening for genital HSV infection in asymptomatic adolescents and adults, including those who are pregnant.
(doi:10.1001/jama.2016.16776; the full report is available pre-embargo to the media at the For the Media website)
Editor’s Note: Please see the article for additional information, including other authors, author contributions and affiliations, financial disclosures, funding and support, etc.
Note: More information about the U.S. Preventive Services Task Force, its process, and its recommendations can be found on the newsroom page of its website.
# # #